Standing up and feeling lightheaded isn’t just a quick spin of the head-it could be your body reacting to a medication you’re taking. This isn’t normal aging. It’s orthostatic hypotension, a sudden drop in blood pressure when you rise from sitting or lying down. For many people, especially those on multiple prescriptions, this isn’t a rare glitch-it’s a daily risk. And it’s more common than you think.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension happens when your blood pressure falls by more than 20 mm Hg systolic or 10 mm Hg diastolic within three minutes of standing. That’s the clinical standard, confirmed by the Merck Manual and the American Academy of Family Physicians. It’s not just a feeling of dizziness-it’s your brain briefly not getting enough blood. Symptoms include blurred vision, nausea, weakness, and sometimes fainting. In older adults, it’s often the reason behind unexplained falls.What makes this dangerous isn’t the dizziness itself. It’s what follows: fractures from falls, hospitalizations, loss of independence, and even increased risk of death over time. Studies show people with this condition have a 24-32% higher chance of dying within 10 years compared to those without it.
Medications Are the Top Culprit
While orthostatic hypotension can come from nerve damage or dehydration, the most common cause in everyday practice is medication. Up to 30% of all cases are directly tied to drugs. And it’s not just one or two-it’s entire classes of commonly prescribed medicines.Here are the big offenders:
- Antihypertensives-Blood pressure pills like diuretics (hydrochlorothiazide), ACE inhibitors (lisinopril), and beta-blockers are meant to lower BP. But sometimes they lower it too much when you stand.
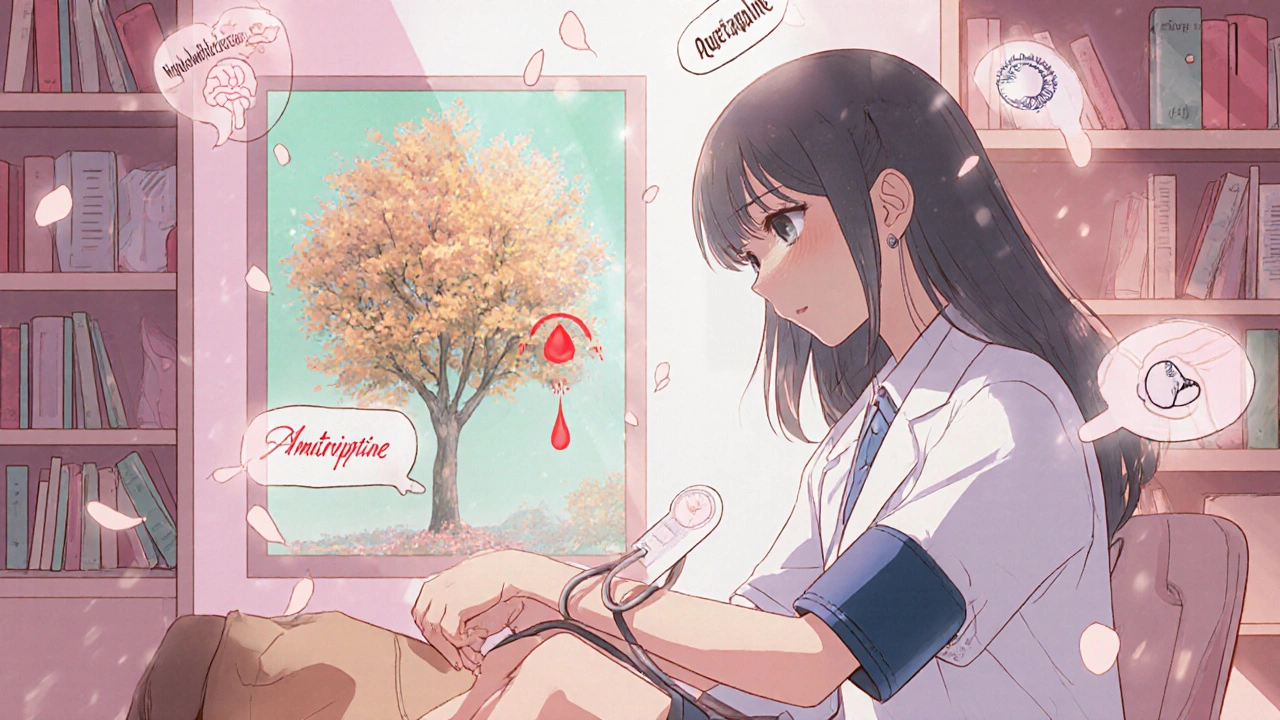
- Antipsychotics-Drugs like quetiapine, clozapine, and chlorpromazine block adrenaline receptors. This can shut down your body’s natural response to standing. Up to 40% of people on these meds experience dizziness on standing.
- Tricyclic antidepressants-Medications like amitriptyline interfere with the autonomic nervous system. They carry a 3.2 times higher risk of causing orthostatic hypotension than other antidepressants.
- Opioids-Morphine, oxycodone, and hydrocodone can cause OH in 15-25% of elderly users. The risk doubles if combined with alcohol or benzodiazepines.
- Levodopa-Used for Parkinson’s, it affects blood pressure control in 30-50% of patients.
- Alpha-blockers-Used for prostate issues (like tamsulosin), these relax blood vessels and can cause sudden drops in BP. Risk is 2.8 times higher than average.
What’s worse? Many people take several of these at once. The average patient with medication-induced orthostatic hypotension is on 6.2 different drugs. And if you’re over 70, your risk jumps 3.2 times. Take four or more medications? Your risk shoots up nearly sixfold.
How It Works: Your Body’s Failed Response
When you stand, gravity pulls blood down into your legs. Normally, your body reacts instantly: your heart beats faster, your blood vessels tighten, and your blood pressure stays steady. This is called the baroreceptor reflex.Medications break this system. Some block adrenaline signals. Others drain fluid from your body. Some depress your brain’s ability to trigger the reflex. The result? Blood pools in your lower body. Your brain gets less oxygen. You feel dizzy-or worse, black out.
Here’s the key difference: if OH is caused by nerve damage (neurogenic), your heart won’t speed up when you stand. If it’s from dehydration, your heart will race. But with drug-induced OH, the pattern is often inconsistent-because the drug is interfering at different points in the system.
Real Stories, Real Consequences
On patient forums and Reddit, the same stories keep appearing:- A 72-year-old woman started quetiapine for anxiety. Within three weeks, she fainted twice when standing up. Her blood pressure dropped from 128/82 to 92/61 in under two minutes.
- A man on hydrochlorothiazide and lisinopril for high blood pressure kept falling. After his doctor stopped the diuretic, his dizziness vanished in 72 hours.
- A 68-year-old on oxycodone for back pain started feeling faint every morning. He didn’t connect it to the painkiller until he lost his balance getting out of bed.
One Mayo Clinic survey found that 55% of patients had symptoms for over two months before anyone linked them to their meds. That’s two months of near-falls, fear, and lost confidence.
Diagnosis: It’s Not as Simple as Asking
Doctors don’t always check for this. Many assume dizziness is just old age. But diagnosing it is simple-if you know how.The standard test: lie down for five minutes. Then stand up. Measure your blood pressure at 0, 1, 2, and 3 minutes after standing. A drop of 20/10 or more confirms orthostatic hypotension. And it must match your symptoms.
Here’s the catch: up to 40% of people with this condition have no symptoms at all. They’re walking around with low BP on standing and don’t even know it. That’s why screening is critical for anyone over 65 or on multiple meds.
Since 2022, the American Geriatrics Society Beers Criteria has listed 12 high-risk medications for seniors. More than two-thirds of U.S. primary care clinics now screen for OH during annual checkups.
What You Can Do: Immediate Steps
You don’t have to live with this. The good news? Medication-induced orthostatic hypotension is often reversible.Here’s what works:
- Review your meds with your doctor. Don’t stop anything on your own. But ask: "Could any of these be causing my dizziness?" Focus on the big offenders: diuretics, antipsychotics, tricyclics, alpha-blockers.
- Stand up slowly. Sit on the edge of the bed for 30 seconds before standing. Hold onto furniture. Don’t rush.
- Drink more water. Aim for 2-2.5 liters a day. Dehydration makes OH worse. Especially in hot weather or if you’re sweating.
- Wear compression stockings. These help push blood back up from your legs. They’re not glamorous-but they work.
- Avoid alcohol and large meals. Both can drop your BP further.
- Elevate the head of your bed. A 6-10 inch raise helps reduce nighttime fluid shifts that worsen morning dizziness.
Studies show 65-80% of patients improve significantly after adjusting medications. In one Stanford Healthcare follow-up, 78% of patients saw major symptom relief within 1-2 weeks of stopping or reducing a culprit drug.
When Medication Adjustment Isn’t Enough
If lifestyle changes don’t help, your doctor might consider medication. Midodrine is the only FDA-approved drug specifically for orthostatic hypotension. It tightens blood vessels. A typical dose is 10 mg three times a day. It reduces symptoms by about 65% in clinical trials.But it’s not for everyone. It can raise BP too much when lying down. That’s why it’s only used after other options are tried.

What’s Changing in Medicine
The field is waking up. In 2020, the FDA started requiring drug labels to include orthostatic hypotension risk if it occurs in more than 5% of trial participants. That’s why you now see warnings on antipsychotics, opioids, and antidepressants.Pharmaceutical companies are developing new drugs designed to avoid this side effect. Seven are currently testing alpha-1A selective agonists-medications that target blood vessels more precisely, reducing the chance of dizziness.
Future research is looking at genetic markers to predict who’s most likely to develop OH from certain drugs. Personalized prescribing is coming.
Why This Matters More Than Ever
By 2040, over 80 million Americans will be over 65. That’s a massive increase in people at risk. OH-related falls cost Medicare $31 billion in 2022 alone. And 30-40% of those costs come from drug-induced cases.This isn’t just about feeling dizzy. It’s about staying independent. Avoiding hospital stays. Living without fear of falling. Every medication has a benefit-but not every benefit outweighs the risk.
If you or someone you care for is on multiple drugs and feels lightheaded when standing, don’t ignore it. Talk to your doctor. Ask for a medication review. It could change everything.
Can orthostatic hypotension go away after stopping a medication?
Yes, in most cases. About 70-85% of people see symptoms improve or disappear completely after stopping or reducing the medication causing the problem. The timeline varies-some feel better in a few days, others take a couple of weeks. It depends on the drug, how long it was taken, and the person’s overall health. Diuretics and alpha-blockers often resolve quickly, while antipsychotics may take longer due to their effects on the nervous system.
Is orthostatic hypotension dangerous if I don’t faint?
Absolutely. You don’t have to faint for it to be dangerous. Even mild dizziness increases your risk of falling, which can lead to broken hips, head injuries, or long-term disability. Studies show people with this condition-even without syncope-have a 24-32% higher risk of death over 10 years. The brain doesn’t get enough blood, and over time, that can affect cognition and heart health. Don’t wait for a fall to take it seriously.
Which medications are safest for seniors who need blood pressure control?
Calcium channel blockers like amlodipine and certain ARBs like losartan tend to have lower rates of orthostatic hypotension compared to diuretics or ACE inhibitors. Beta-blockers are also less likely to cause it than alpha-blockers. But the safest choice depends on your other conditions-like heart failure, kidney disease, or diabetes. Always ask your doctor: "Is there a similar medication with a lower risk of dizziness?"
Can I still take my antidepressant if it causes dizziness?
It depends. Tricyclic antidepressants like amitriptyline have a high risk of causing OH-3.2 times higher than other types. If you’re on one and feeling dizzy, talk to your doctor about switching to an SSRI like sertraline or escitalopram, which are much less likely to cause this side effect. Never stop abruptly. Your doctor can help you taper safely while managing your mental health.
Why do I feel dizzy only in the morning?
Morning dizziness is common because your body has been lying flat all night, and fluids have pooled in your lower body. If you’re on a diuretic taken at night, you may be slightly dehydrated when you wake up. Also, your blood pressure naturally dips overnight. Standing up right away causes a bigger drop. Try drinking a glass of water before getting up, sitting on the edge of the bed for a minute, and moving slowly.
Should I avoid standing up quickly even if I’m not on meds?
Yes, it’s a good habit for everyone, especially after 50. Your body’s ability to regulate blood pressure slows with age-even if you’re not on medication. Standing too fast can cause temporary dizziness in healthy people. Making it a routine to rise slowly protects you now and prepares you for future changes. It’s simple, free, and reduces fall risk by up to 30%.
Can compression stockings help even if I’m not elderly?
Yes. Compression stockings work by squeezing your legs to push blood back toward your heart. They’re not just for older adults. People with prolonged standing jobs, those recovering from illness, or even younger adults on certain medications can benefit. Look for medical-grade stockings with 15-20 mm Hg pressure. Wear them from morning until bedtime, and remove them before sleeping.
Next Steps: What to Do Today
If you’re on multiple medications and feel dizzy when standing:- Write down every drug you take-including vitamins and supplements.
- Track when the dizziness happens: after meals? In the morning? After standing up fast?
- Measure your blood pressure at home: sit for 5 minutes, then stand and measure again at 1 and 3 minutes.
- Book an appointment with your doctor. Ask: "Could any of my meds be causing orthostatic hypotension?"
- Start drinking more water and stand up slowly.
You don’t need to accept dizziness as normal. With the right steps, you can feel steady on your feet again.


Peter Aultman
November 13, 2025 AT 04:42Been dealing with this since I started lisinopril last year. Didn’t realize it was the med until I stopped for a week and suddenly didn’t feel like I was gonna pass out every time I got up. Simple fix. Just didn’t know to ask.
Now I sit for 30 seconds like the post says. Life’s better.
Sean Hwang
November 15, 2025 AT 02:13My grandma was on 7 meds and kept falling. Doctor said it was just old age. Took us 6 months to get someone to check her orthostatic bp. She dropped 3 meds, started compression socks, and now walks the neighborhood every morning. No more ER trips.
Don’t let them brush it off. This stuff is fixable.
Kevin Wagner
November 15, 2025 AT 08:46THIS IS WHY WE NEED TO STOP TREATING SENIORS LIKE BROKEN VACUUMS. You don’t just ‘get old’ and suddenly become a walking hazard. Someone gave your grandma a cocktail of drugs that tanked her BP and now you’re told to just ‘be careful’? That’s not care. That’s negligence.
Doctors need to stop prescribing like they’re playing Russian roulette with a full magazine. We’re not talking about a little dizziness-we’re talking about broken hips, dementia from repeated head trauma, and early death. This isn’t a side effect. It’s a systemic failure.
And yes, I’ve seen it. My uncle died after a fall from quetiapine. He never even knew it was the meds. They didn’t even test him. They just wrote it off as ‘senior moments.’
Stop normalizing this. Demand a med review. Every. Single. Time.
Don Ablett
November 16, 2025 AT 21:28The clinical definition of orthostatic hypotension is well established but often overlooked in primary care settings. The baroreceptor reflex is a complex autonomic response and pharmacologic interference is frequently underestimated. A 2021 JAMA study indicated that up to 41% of patients on polypharmacy regimens exhibited asymptomatic orthostatic hypotension. Screening protocols remain inconsistent across institutions despite Beers Criteria recommendations. Further research into pharmacogenomic predictors is warranted to mitigate adverse outcomes in vulnerable populations.
It is imperative that clinicians adopt standardized BP measurement protocols upon standing rather than relying on patient self-reporting alone.
Compression stockings remain an underutilized nonpharmacologic intervention with demonstrated efficacy in randomized trials.
Jane Johnson
November 17, 2025 AT 05:23Interesting how everyone blames the meds. What about the patients who refuse to stand slowly? Or drink water? Or wear socks? It’s not always the doctor’s fault.
People just want to be told their meds are the problem so they don’t have to change anything.
And why do you all assume every elderly person is helpless? I’m 73 and I’ve never had this issue. Maybe it’s not the drugs. Maybe it’s laziness.
gent wood
November 18, 2025 AT 08:25I’ve been a nurse for 22 years and I’ve seen this exact scenario play out a hundred times. A patient comes in saying they feel faint when they stand. The doctor says, ‘You’re getting older.’ No BP check. No med review. No questions.
Then six months later, they’re in rehab after a hip fracture.
It’s not just about the drugs-it’s about the system. We’re treating symptoms, not causes. We’re prescribing like we’re filling a grocery list, not managing a human body.
And the worst part? The patients don’t know to ask. They think dizziness is just part of life.
So thank you for writing this. Someone needed to say it out loud.
And to Jane-yes, some people are lazy. But most are just scared, confused, and told for years that it’s normal. They need guidance, not judgment.
Dilip Patel
November 18, 2025 AT 13:25USA doctors are so stupid they give old people 7 drugs and then say its age. In india we just give one pill and tell them to walk. No dizziness. No problem. You people overmedicate everything. My uncle had high bp and doctor gave him 5 pills. He fell 3 times. I took him to local clinic. They gave him one tablet and said drink water and walk. He’s fine now. You need to stop being so complicated. Simple things work. Why you make it hard? Also compression socks? Why not just stand slow? Its free. No need to buy fancy stuff. Also why you all so scared to die? Just sit down if you feel dizzy. No big deal. You think you are special? Everyone gets dizzy. Just live with it.
Barry Sanders
November 19, 2025 AT 13:38Wow. Another ‘meds are evil’ sob story. Let me guess-you didn’t even check your blood pressure before assuming it’s the drugs. Or maybe you just want an excuse to stop taking your pills.
Orthostatic hypotension isn’t a conspiracy. It’s a physiological response. Maybe you’re dehydrated. Maybe you’re sedentary. Maybe you’re just bad at standing up.
And compression stockings? Really? You’re 45 and you need medical gear to stand? Pathetic.
This post reads like a pharmaceutical ad disguised as medical advice. Wake up. The real problem is people who think their body is a machine that breaks when they take a pill. It’s not. It’s adaptable. You just need to move more, drink more, and stop whining.