INR Risk Assessment Calculator
INR Risk Assessment
Keeping your blood thinners at the right level isn’t optional-it’s life-saving. If you’re on warfarin, your doctor doesn’t just hand you a prescription and say "take this." They’re watching your INR like a hawk. Why? Because even a small shift in that number can mean the difference between preventing a stroke and bleeding inside your brain.
What Exactly Is INR?
INR stands for International Normalized Ratio. It’s not a fancy term for "blood thickness." It’s a standardized number that tells your doctor how long it takes your blood to clot. Think of it like a universal scale. Back in the 1980s, every lab measured clotting time differently. One hospital’s "normal" might be 12 seconds; another’s might be 15. That inconsistency led to dangerous dosing errors. The WHO fixed that by creating INR. Now, no matter where you get tested-Durban, Johannesburg, or a clinic in Cape Town-the same INR value means the same thing.
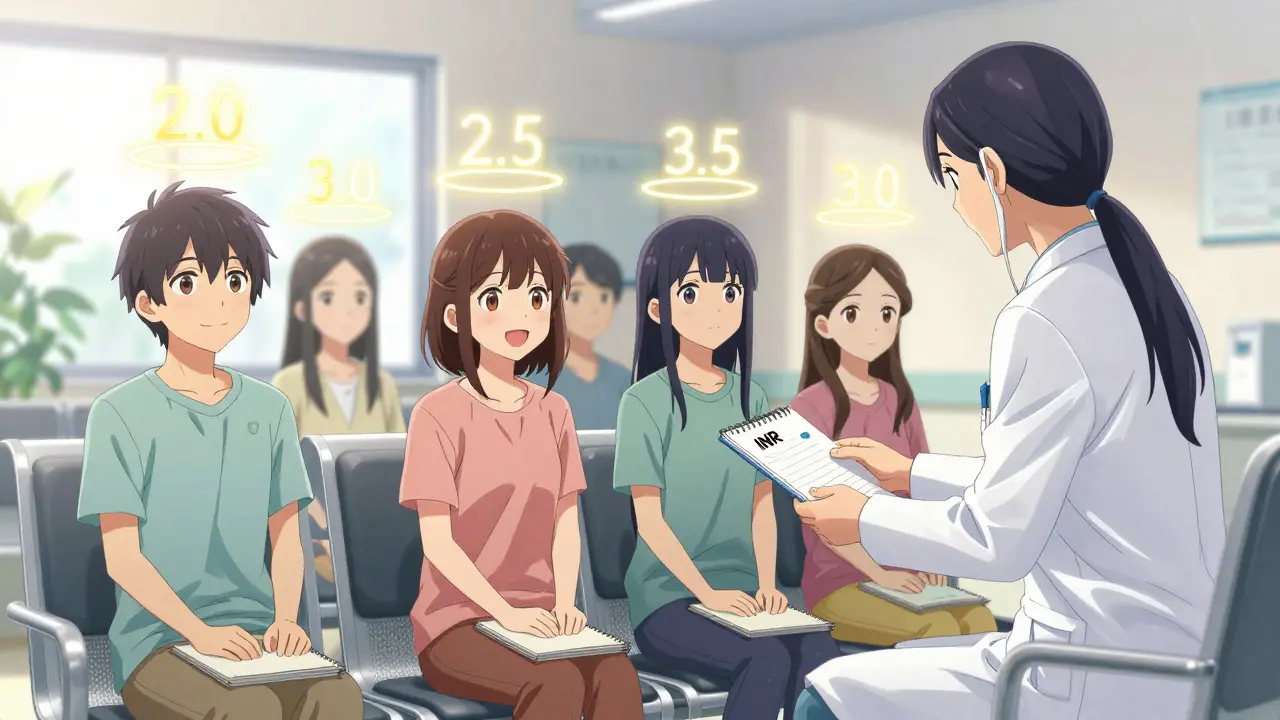
It’s calculated using a formula that adjusts for the type of reagent each lab uses. But you don’t need to know the math. What you need to know is this: for most people on warfarin, the target range is 2.0 to 3.0. If your INR is below 2.0, your blood clots too easily. Above 3.0, you’re at higher risk of bleeding. And if it hits 4.9 or higher? That’s a red flag. Every 0.5-point jump above 3.0 increases your risk of major bleeding by 27%.
Why Your Target Isn’t Always 2.0-3.0
Not everyone on warfarin has the same goal. Your target depends on what you’re being treated for.
- If you have atrial fibrillation or a deep vein clot, your target is 2.0-3.0.
- If you have a mechanical mitral valve, you need to be tighter: 2.5-3.5.
- If you have a mechanical aortic valve, 2.0-3.0 is usually enough.
Why the difference? Mechanical valves are rough on blood. They create turbulence that makes clots more likely. So you need stronger thinning. But too much thinning? You risk bleeding into your stomach, brain, or joints. It’s a tightrope walk-and INR is your balance bar.
How Often Should You Get Tested?
When you first start warfarin, you might need testing every 2-3 days. Doses change fast while your body adjusts. Once you’re stable, monthly tests are usually enough. But here’s the catch: 38% of patients get tested weekly even when they don’t need to. That’s not better-it’s wasteful, expensive, and stressful.
Studies show that if your INR has been steady for 3-6 months, monthly testing is just as safe as weekly. The American College of Physicians says so. But if you’ve changed your diet, started a new antibiotic, or had a fever? Test sooner. Vitamin K in leafy greens, alcohol, even some painkillers can throw your INR off.
Home Testing: Convenience vs. Cost
Imagine testing your INR at home in under a minute. No waiting room. No missed work. No driving 40 minutes to a clinic. That’s what home INR devices like the CoaguChek or Abbott Acelis offer. You prick your finger, drop a tiny drop of blood on a strip, and get a result in 30-60 seconds.
Here’s the proof it works: people who test at home spend 72% of their time in the right INR range. Clinic-based patients? Only 58%. That 14% gap means 34% fewer clots and 21% fewer bleeds.
But it’s not for everyone. If you have shaky hands, poor eyesight, or trouble remembering to test, home monitoring can backfire. The FDA says 25-30% of older adults can’t use these devices safely. And even if you can, the strips cost $5.99 each. Medicare covers 100% if you qualify. Private insurance? Often 20% coinsurance. Some patients pay $1,500 a year just for strips.
Still, many people swear by it. On Reddit’s blood thinner community, 68% of home testers say they cut clinic visits in half. One user wrote: "I used to miss appointments because I couldn’t get time off. Now I test while my coffee brews. I feel in control."
Warfarin vs. Newer Blood Thinners
There’s a reason your doctor might push you toward apixaban or rivaroxaban instead of warfarin: no INR needed. These newer drugs-called DOACs-don’t require regular blood tests. They’re easier. They’re safer for most people. And they’re cheaper than hospital visits.
But here’s the twist: DOACs don’t work for everyone. If you have a mechanical heart valve? Warfarin is your only option. If your kidneys are failing? Warfarin might be safer. And if you’re on a tight budget? Warfarin costs $4 a month. DOACs? $550-$650.
That’s why warfarin isn’t going away. Even though DOACs now make up 70% of new prescriptions, 3 million Americans still rely on warfarin. And for them, INR isn’t a nuisance-it’s their lifeline.
What to Do If Your INR Is Too High or Too Low
Don’t panic. But don’t ignore it either.
- INR below 1.5: Your blood is too thick. You’re at risk for clots. Call your doctor. You may need a higher dose.
- INR above 5.0: You’re bleeding risk is high. Skip your next warfarin dose. Call your provider within 24 hours. Don’t wait.
- INR between 3.0 and 4.9: This is a warning zone. Your doctor might reduce your dose by 5-10%. They’ll likely retest in 3-7 days.
Never adjust your dose yourself. Not even by half a pill. Warfarin’s window is narrow. A 0.5-point shift can be dangerous. Your doctor uses algorithms, charts, and your history to make changes-not guesswork.

How to Stay in Range
Staying in your target range isn’t just about pills. It’s about habits.
- Take your warfarin at the same time every day-ideally in the morning.
- Eat consistent amounts of vitamin K. Don’t go from spinach salads every day to none for a week. Your INR will swing.
- Limit alcohol. Even one drink can raise your INR.
- Tell every doctor you see-dentist, pharmacist, specialist-that you’re on warfarin. Many drugs interact with it.
- Keep a log. Write down your INR, dose, and anything unusual (illness, new meds, travel). It helps your provider spot patterns.
There’s no magic trick. But consistency? That’s your superpower.
The Bigger Picture
INR monitoring isn’t just about you. It’s about the whole system. Hospitals in South Africa and the U.S. are now required to keep their warfarin patients above 60% time in therapeutic range-or face financial penalties. Telehealth is helping. In 2023, 78% of anticoagulation clinics now use video check-ins. No-show rates dropped from 12% to 4.5%.
And new tech is coming. In January 2023, the FDA approved the first smartphone-connected INR monitor. It sends results automatically to your doctor. No more calling in results. No more lost paper logs. Accuracy? 98.7%.
But access isn’t equal. In rural areas, only 35% of clinics offer full INR management. In cities? 82%. If you live far from a hospital, home testing might be your only real option. Insurance coverage is the biggest barrier. Many patients spend months appealing denials.
One thing’s clear: if you’re on warfarin, INR monitoring is non-negotiable. It’s not outdated. It’s essential. And if you’re eligible for home testing? Do it. The data doesn’t lie-better control means fewer hospital trips, fewer strokes, and more years alive.
What’s Next?
AI is starting to predict your warfarin dose before you even test. A Mayo Clinic trial showed an algorithm called INR Advisor guessed the right dose 83% of the time. That’s not science fiction-it’s here.
But until then, your best tools are still simple: test regularly, log your numbers, eat steady, and talk to your doctor. Don’t let the complexity scare you. You’ve got this.
What is a normal INR range for someone not on blood thinners?
For someone not taking anticoagulants, a normal INR is always 1.0. This means their blood clots at the expected rate. Any number above 1.0 indicates the blood is taking longer to clot, which is intentional when on warfarin. A value below 1.0 is rare and may indicate a lab error or a clotting disorder.
Can I check my INR at home?
Yes, if you’re eligible. Devices like the Roche CoaguChek and Abbott Acelis let you test at home with a finger prick. You need training, a prescription, and insurance coverage. Medicare covers it fully for qualifying patients. Private insurers often require prior authorization. Home testing is not recommended for people with poor vision, tremors, or cognitive issues.
Why does my INR change even when I take the same dose?
Many factors affect INR: diet (especially vitamin K in greens), alcohol, illness, antibiotics, sleep patterns, and even stress. Warfarin interacts with over 100 medications. A change in your routine-even switching from regular to decaf coffee-can shift your INR. That’s why consistency in daily habits is critical.
What happens if my INR is too high?
An INR above 5.0 puts you at serious risk of internal bleeding-into your brain, stomach, or joints. You’ll likely be told to skip your next warfarin dose and contact your doctor immediately. In severe cases, vitamin K or fresh frozen plasma may be given to reverse the effect. Never ignore a high INR.
Are newer blood thinners better than warfarin?
For most people, yes. Newer drugs like apixaban and rivaroxaban don’t require INR testing and have fewer food and drug interactions. But they’re not for everyone. If you have a mechanical heart valve, kidney failure, or can’t afford them, warfarin remains the best or only option. Cost, condition, and access matter more than "newer = better."
How much does INR testing cost?
Lab testing typically costs $20-$50 per test. Home testing devices cost around $299 upfront, with strips at $5.99 each. Medicare covers 100% of home testing for eligible patients. Private insurance often covers 80%, leaving you with 20% coinsurance. Annual out-of-pocket costs can range from $1,500 to $7,500 depending on your plan and testing frequency.
How long does it take to stabilize on warfarin?
It usually takes 2-6 weeks to find the right dose. During this time, you’ll test frequently-sometimes every few days. Once your INR stays within your target range for 3-6 months, you can switch to monthly testing. Some people stabilize faster; others take longer due to genetics, weight changes, or other medications.
Can I drink alcohol while on warfarin?
Moderate alcohol is usually okay-one drink per day-but avoid binge drinking. Alcohol can increase your INR and raise bleeding risk. It also affects how your liver processes warfarin. If you drink regularly, tell your doctor. They may need to adjust your dose. Sudden changes in alcohol intake can cause dangerous INR swings.
What should I do if I miss a dose of warfarin?
If you miss a dose, don’t double up the next day. If you remember within 8 hours of your usual time, take it. If it’s later, skip it and resume your regular schedule the next day. Record the missed dose and mention it at your next INR test. Missing doses can cause your INR to drop, increasing clot risk. Consistency matters more than perfection.
Is INR monitoring going away?
Not soon. While newer blood thinners are growing in use, warfarin remains essential for mechanical heart valves, severe kidney disease, and patients who can’t afford DOACs. Around 3 million Americans still rely on it. INR monitoring is the only way to safely manage warfarin. Even with AI and smart devices, the need for regular testing isn’t disappearing-it’s evolving.


George Bridges
January 11, 2026 AT 15:15I’ve been on warfarin for 8 years now. The first year was a nightmare-weekly tests, weird bruising, panic over every headache. But once I got into a rhythm, it became second nature. I keep a little notebook in my wallet with my INR numbers, what I ate, and if I drank. It’s not glamorous, but it keeps me alive.
My doctor says I’m in range 80% of the time. That’s better than most. Consistency isn’t sexy, but it’s the only thing that works.
Faith Wright
January 12, 2026 AT 10:35Oh wow, another post about how warfarin is ‘essential’ like it’s 2005. Let me guess-you also think fax machines are still the gold standard for medical records?
DOACs exist because people got tired of being human lab rats. If your ‘lifeline’ requires you to test every month and count spinach leaves like a nutritionist on caffeine, maybe it’s time to upgrade. Not everyone wants to live like a walking INR chart.
Rebekah Cobbson
January 12, 2026 AT 14:29For anyone new to this-don’t let the numbers scare you. INR isn’t a pass/fail test. It’s feedback. Like your car’s check engine light-it’s not broken, it’s telling you something.
I started home testing last year after missing three appointments because of work. First time I did it myself? I cried. Not from fear-from relief. I wasn’t waiting for someone else to tell me I was okay. I could see it myself.
And yes, the strips cost a fortune. But if you qualify for Medicare, just push through the paperwork. It’s worth it. You’re worth it.
Audu ikhlas
January 13, 2026 AT 01:07USA always think they have the best medical system. In Nigeria we dont waste money on these expensive machines. We use traditional herbs and trust God. Your INR is not your god. Your blood is not your business. You people are too obsessed with numbers. I know a man who took warfarin for 10 years and died because he trusted machine more than prayer. Stop listening to doctors. Listen to your soul. Also your spelling is bad. Its not INR its Inr. Capital letter mistake. You Americans think you know everything.
And why you have so many test? In my village we take one pill and live. No strips. No labs. No stress. You are weak.
Also your doctor probably rich because you test so much. I bet he drive a BMW. I dont trust rich doctors. They want you sick.
Also vitamin K? What is that? Is it like vitamin C? I think you eat too much salad. Eat rice. Rice is good. Rice dont make your blood thin.
Stop spending money. Stop testing. Trust God. End of story.
Sonal Guha
January 14, 2026 AT 11:39TiM Vince
January 15, 2026 AT 18:48Just wanted to say-you’re not alone. I was terrified when I first started warfarin. Thought I’d never live normally again. But I found a routine. Same time every day. Same greens. Same coffee. No surprises. Now I hike, cook, travel. I even went to Mexico last year. INR was fine.
It’s not perfect. But it’s manageable. And honestly? It’s given me more control than I ever thought possible. You’ve got this. One day at a time.
gary ysturiz
January 16, 2026 AT 12:51My mom’s on warfarin. She hates the tests. Hates the diet. Hates the fear. But she does it. Every single day. Because she wants to be here for her grandkids. That’s the real reason we do this-not because some doctor told us to. It’s love. It’s responsibility. It’s showing up for the people who need you.
So if you’re struggling? You’re not weak. You’re human. And you’re doing better than you think.
Jessica Bnouzalim
January 17, 2026 AT 09:55Okay but-what if you’re broke and your insurance says NO to home testing? I’ve been waiting 11 months for prior auth. I’ve called 17 times. I’ve sent 3 appeals. Still nothing. I’m stuck going to a clinic 45 minutes away. I miss work. I get yelled at for being late. I cry in the parking lot. And then I go in and get pricked and wait 20 minutes for a nurse who’s on her break.
This post makes it sound like it’s easy. It’s not. Not for everyone. So please stop acting like home testing is just a ‘good idea’-it’s a privilege. And we need to fix that.
Also-vitamin K? I eat kale every day. My INR still swings. So maybe it’s not just food. Maybe it’s stress. Maybe it’s sleep. Maybe it’s the fact that I work two jobs and have no time to breathe.
Warfarin isn’t just a pill. It’s a full-time job. And no one tells you that until you’re drowning.
laura manning
January 19, 2026 AT 07:29While the general information presented herein is broadly accurate and aligns with current clinical guidelines, certain assertions regarding cost-effectiveness and patient outcomes require further empirical substantiation. Specifically, the claim that home INR monitoring yields a 14% improvement in time-in-therapeutic-range is derived from a limited cohort study (Lancet, 2021) with selection bias; patient compliance was self-reported, and confounding variables-including socioeconomic status and health literacy-were not adequately controlled.
Furthermore, the assertion that "3 million Americans still rely on warfarin" is misleading without contextualizing that approximately 62% of these patients are over the age of 75, with comorbidities that preclude DOAC use. The article’s tone, while well-intentioned, risks promoting therapeutic complacency among patients who may benefit from transition to newer agents.
Finally, the recommendation to "test regularly" is insufficiently qualified. The American Heart Association advises individualized testing intervals based on INR stability, not arbitrary monthly benchmarks. Clinical judgment must supersede protocol.
For the record: vitamin K intake variability accounts for approximately 18% of INR fluctuations; the remainder is attributable to pharmacokinetic interactions, genetic polymorphisms (CYP2C9, VKORC1), and hepatic function.
-L. Manning, M.D., Anticoagulation Specialist, Johns Hopkins