Milk Thistle Drug Interaction Checker
This tool helps you understand potential interactions between milk thistle and your medications based on current scientific evidence. Remember: Natural doesn't always mean safe.
Millions of people take milk thistle every day for liver support. But if you’re also on prescription meds-especially blood thinners, seizure drugs, or statins-you could be at risk for something you didn’t even know to watch for: milk thistle messing with how your liver processes your drugs.
What Milk Thistle Actually Does in Your Liver
Milk thistle isn’t just a trendy supplement. Its active ingredient, silymarin, is a mix of compounds-mostly silybin-that have been studied for over 60 years. German scientists first noticed it protected the liver in the 1960s. Today, it’s one of the most popular herbal supplements worldwide, with over 38% of the global hepatoprotective market. People take it for fatty liver, alcohol-related liver damage, and even hepatitis. But here’s the catch: it doesn’t just sit there and protect. It talks to your liver’s drug-processing system.
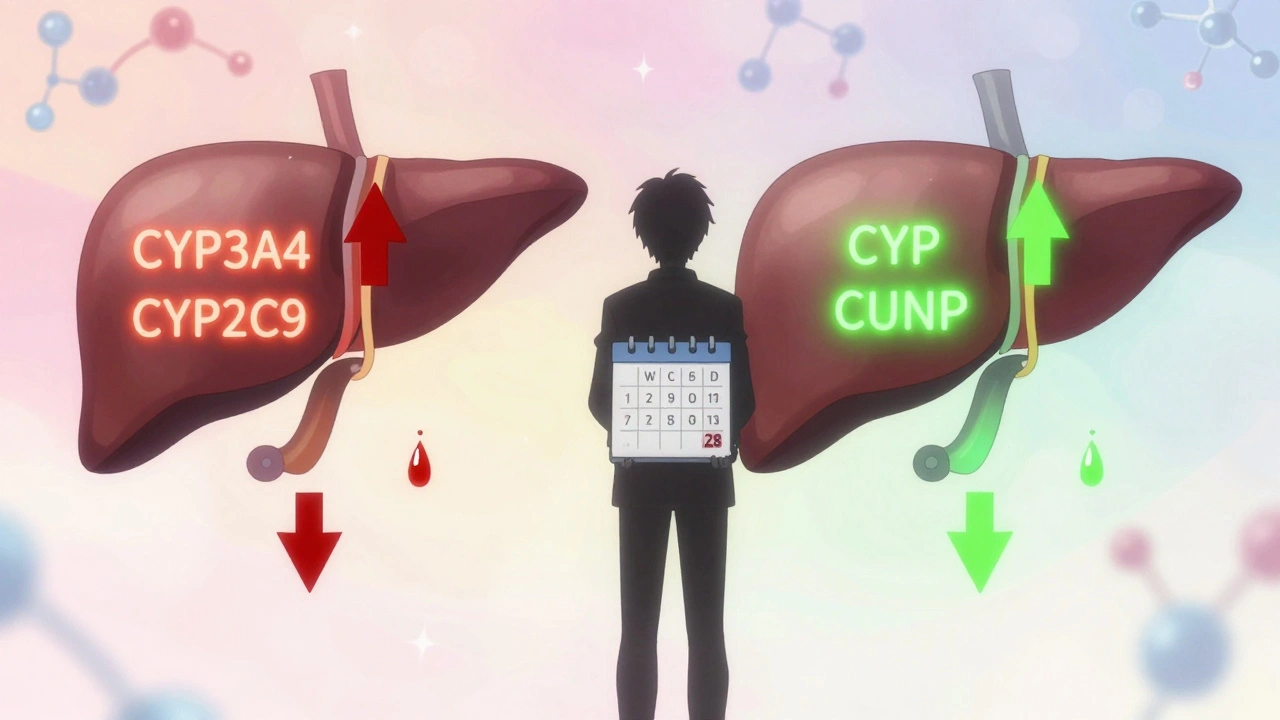
Your liver uses enzymes called cytochrome P450 (CYP) to break down most prescription drugs. The big players here are CYP3A4, CYP2C9, and CYP2D6. These enzymes handle everything from warfarin to statins to antidepressants. Silymarin, the main component in milk thistle, can interfere with these enzymes-but not in a simple, predictable way.
The Confusing Science: Inhibition vs. Induction
Here’s where things get messy. Some studies say milk thistle blocks liver enzymes. Others say it boosts them. And sometimes, it does both-depending on how long you’ve been taking it.
A 2021 lab study showed silymarin reduced CYP2C9 activity by 15-23%. That’s a problem if you’re on warfarin or phenytoin, both metabolized by CYP2C9. If the enzyme slows down, your drug builds up. That can lead to dangerous bleeding or toxicity.
But then, a 2019 clinical trial gave 420 mg of silymarin daily to 24 healthy people for two weeks. No meaningful change in CYP3A4 activity. The drug midazolam, which relies on CYP3A4, stayed in their systems at nearly the same level. So why the contradiction?
Turns out, it’s time-dependent. A 2020 study found that after just a few days, silymarin blocked CYP2C9. But after 28 days, the enzyme started working faster-up by 12.7%. That means your drug could get cleared too quickly, making it less effective. One day, your blood thinner works fine. Two weeks later, it doesn’t. And you don’t know why.
Real People, Real Problems
Science can be abstract. Real life isn’t.
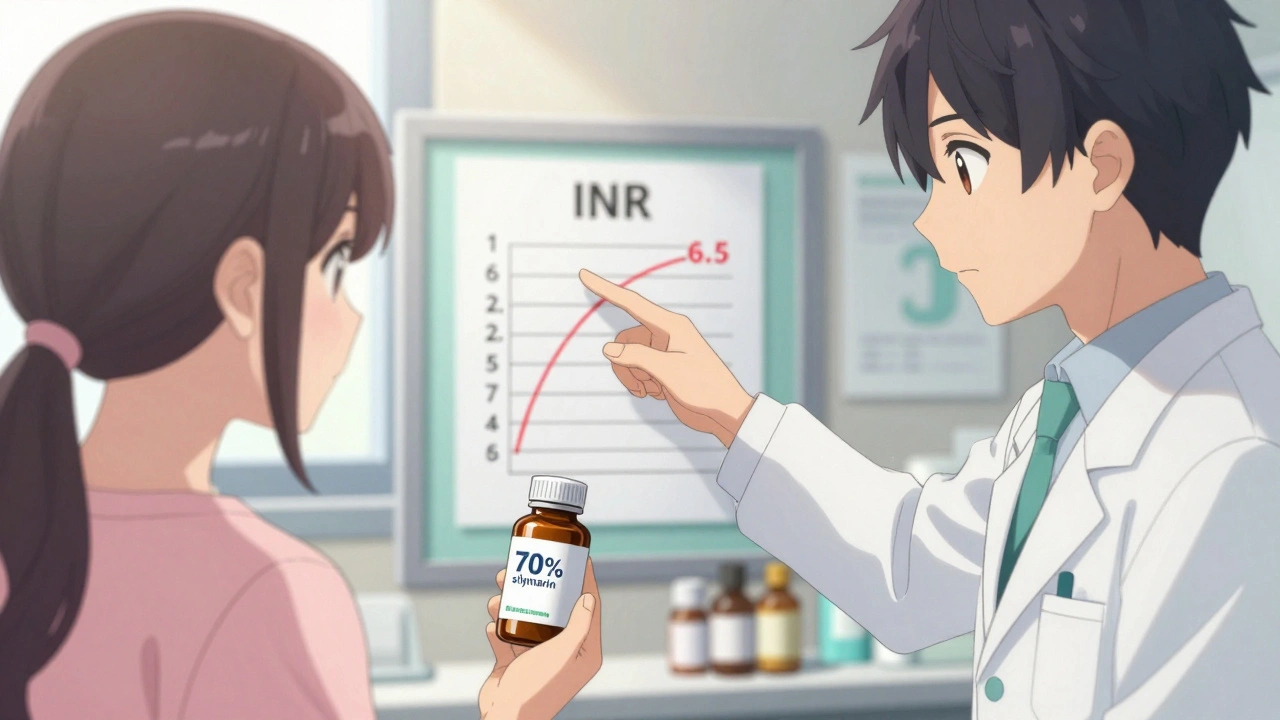
On Reddit, a user posted in February 2024: “I started milk thistle for my fatty liver. Two weeks later, my INR shot up to 6.5. I was hospitalized.” His INR-how long it takes blood to clot-normally hovered around 2.5 on warfarin. After milk thistle, it nearly tripled. He needed an emergency dose of vitamin K and a 30% reduction in his warfarin. He wasn’t alone. Over 40 people in that thread reported the same thing.
But flip to Amazon reviews, and you’ll see mostly glowing feedback. Only 2.1% mentioned drug interactions. Why? Because most people aren’t on warfarin. They’re on a statin or a multivitamin. And for those drugs? Milk thistle might be fine.
One man with hepatitis C took 420 mg of milk thistle daily for 12 weeks alongside sofosbuvir/velpatasvir. No issues. That’s consistent with data showing minimal interaction with direct-acting antivirals. So it’s not that milk thistle is universally dangerous. It’s dangerous for certain drugs in certain people.
Who’s at Risk?
Not everyone needs to avoid milk thistle. But if you’re taking any of these, proceed with extreme caution:
- Warfarin (Coumadin, Jantoven): High risk. Even small changes in CYP2C9 can cause bleeding.
- Phenytoin (Dilantin): Used for seizures. Silymarin can cause levels to spike or crash.
- Statins (atorvastatin, simvastatin): Metabolized by CYP3A4. The risk is theoretical but real enough that 37% of doctors on HealthTap advise caution.
- Immunosuppressants (cyclosporine, tacrolimus): Critical for transplant patients. Small changes can mean rejection.
- Some antidepressants and anti-anxiety meds: Especially those processed by CYP2D6.
People with liver disease are often the ones taking milk thistle-but they’re also the ones most likely to be on multiple meds. That’s a dangerous combo.
What About Quality?
Not all milk thistle is created equal. Only 32% of supplements tested in a 2022 FDA study actually contained the amount of silymarin listed on the label. Some had too little. Some had contaminants. Others had fillers that might affect absorption.
If you’re going to take it, look for standardized extracts with 70-80% silymarin. Avoid “whole herb” powders-they’re unpredictable. And if you’re on a tight budget, cheaper brands aren’t worth the risk. You’re not just buying a supplement. You’re buying a variable that could alter your medication’s effect.
What Do Experts Say?
There’s no consensus. Dr. Joseph Pizzorno, a leading voice in natural medicine, says the risk is overstated. He points to only 12 case reports in 40 years, and none proved milk thistle caused the problem.
Dr. David Bernstein, a top hepatologist, disagrees. He says: “Until we have consistent data, treat milk thistle like a drug-not a vitamin.”
The European Medicines Agency says interactions are unlikely at normal doses. The U.S. NIH’s LiverTox database says it’s “possibly interacting” with CYP2C9 substrates. The FDA doesn’t require supplement labels to warn about drug interactions. So you’re on your own.
What Should You Do?
Here’s the practical guide:
- Don’t start milk thistle without telling your doctor-especially if you’re on any prescription meds.
- If you’re already taking it, get your drug levels checked. For warfarin, check INR weekly for the first month. For phenytoin, check levels at days 3, 7, and 14 after starting.
- Wait 48 hours after stopping milk thistle before testing baseline drug levels. Enzyme effects don’t vanish overnight.
- Don’t assume it’s safe just because it’s “natural.” Natural doesn’t mean harmless.
- Track your symptoms. Unexplained bruising, dizziness, fatigue, or changes in mood could be signs your meds aren’t working right.
If you’re using milk thistle for fatty liver, know this: 65.5% of studies show it improves liver enzymes. But so do weight loss, exercise, and cutting sugar. Those don’t interact with your meds. Why risk it?
The Bigger Picture
The supplement industry is booming. The global market for milk thistle is expected to hit $285 million by 2030. But regulation? Still a mess. In Europe, it’s a licensed medicine. In the U.S., it’s a dietary supplement with no labeling requirements for interactions.
Doctors aren’t trained for this. A 2023 JAMA survey found only 28% of physicians felt confident advising patients on milk thistle-even though over 60% get asked about it.
Meanwhile, researchers are working on new forms of silybin bound to phosphatidylcholine. Early trials suggest these versions may keep the liver benefits without the enzyme interference. But they’re not on shelves yet.
For now, the safest approach is simple: If you’re on meds that your liver processes, treat milk thistle like a drug. Not a vitamin. Not a harmless herb. A substance that can change how your body handles your prescriptions.
Ask your doctor. Get tested. Don’t guess. Your liver might thank you-but your blood, your brain, and your safety? They’ll thank you more.


Ali Bradshaw
December 4, 2025 AT 19:59I’ve been taking milk thistle for my fatty liver for about a year now. Never thought about drug interactions until I read this. I’m on a low-dose statin and just checked with my pharmacist-she said it’s probably fine, but to watch for muscle fatigue. Good reminder to not assume ‘natural’ means ‘safe.’
an mo
December 6, 2025 AT 10:04Let’s cut through the woo. This isn’t ‘herbal medicine’-it’s an unregulated, poorly studied compound with enzyme-modulating effects that even the FDA won’t require labels for. If you’re on warfarin and you’re popping milk thistle like it’s a gummy vitamin, you’re playing Russian roulette with your coagulation cascade. Stop being naive. This isn’t tea-it’s a pharmacokinetic wildcard.
aditya dixit
December 7, 2025 AT 12:11There’s a deeper truth here: we treat supplements like they exist outside of biology. But the liver doesn’t care if something is ‘natural’ or ‘synthetic.’ It only cares about molecular structure and enzyme affinity. Silymarin is a ligand. It binds. It competes. It alters. The science isn’t contradictory-it’s dynamic. The body adapts. That’s why timing matters. Two weeks in, you’re inhibited. Four weeks in, you’re induced. It’s not a bug-it’s a feature of human physiology.
Maybe the real problem isn’t milk thistle. It’s that we’ve outsourced our health literacy to marketing departments and Amazon reviews.
Annie Grajewski
December 7, 2025 AT 16:32so like… milk thistle is basically the herbal version of that one friend who shows up to your party and then messes with your playlist? one minute you’re chillin’ with your warfarin bops, next thing you know your INR’s at 6.5 and you’re in the ER listening to some nurse say ‘uhhh… did you take anything weird?’ yeah. i took the ‘liver cleanse’ gummies. my bad.
Marvin Gordon
December 9, 2025 AT 03:37This is exactly why I stopped taking any supplement without talking to my doctor first. I was on simvastatin and started milk thistle because my cousin swore by it. Two weeks later, I had unexplained bruising on my arms. Got my INR checked-was borderline dangerous. I stopped the milk thistle immediately. My doctor said I was lucky. Don’t be like me. Ask first.
Norene Fulwiler
December 9, 2025 AT 13:49As someone who grew up in a family that trusts herbs more than pills, this hit hard. My mom’s been on milk thistle since 2018. She’s on blood pressure meds and thyroid med. I’ve been begging her to get her levels checked. She says ‘it’s just a plant.’ But plants are powerful. This post made me finally send her the link. I hope she listens.
William Chin
December 11, 2025 AT 01:27It is imperative to underscore that the absence of regulatory oversight in the dietary supplement industry constitutes a profound public health vulnerability. The lack of mandatory interaction warnings on milk thistle products represents a systemic failure of consumer protection mechanisms. One must exercise the utmost prudence and seek formal pharmacological consultation prior to ingestion of any phytochemical agent possessing documented cytochrome P450 modulatory properties.
Katie Allan
December 11, 2025 AT 10:33I’ve been a nurse for 18 years and I’ve seen too many patients assume herbal = harmless. I’ve had people come in with bleeding ulcers because they started turmeric and milk thistle while on aspirin. This post should be required reading for anyone over 40 who’s on meds. Please, if you’re reading this and you’re taking something ‘natural’-tell your doctor. No judgment. Just safety.
Deborah Jacobs
December 12, 2025 AT 12:18My grandma used to say, ‘If it’s got a name you can’t spell, it’s got a price you can’t afford.’ Milk thistle? Sure. But when your meds are running on a liver that’s now confused by a plant trying to be a pharmacy? That’s when you start sweating. I started tracking my INR like a journal after this. Now I write down everything I put in my mouth-even the ‘harmless’ stuff. My blood thinner doesn’t care if it’s organic. It just cares if it works.
Lucy Kavanagh
December 12, 2025 AT 17:17Did you know the FDA doesn’t test supplements? That’s why big pharma doesn’t want you to know this-milk thistle is a Trojan horse. They let it slide because if people start asking questions about what’s in their ‘natural’ pills, they’ll start asking about the drugs too. And then… the whole system cracks. You think this is about liver health? Nah. It’s about control. Don’t be fooled.