Switching from a generic medication back to the brand-name version isn’t as simple as asking your pharmacist for the original pill. It’s a medical decision-with real risks, legal steps, and insurance hurdles-that needs to be handled carefully. Many people assume generics and brand drugs are identical, but that’s only true for the active ingredient. The rest? Fillers, dyes, coatings, and binders can vary wildly. And for some people, those differences cause real problems.
Why You Might Need to Switch Back
- You developed a rash, nausea, or allergic reaction after switching to the generic.
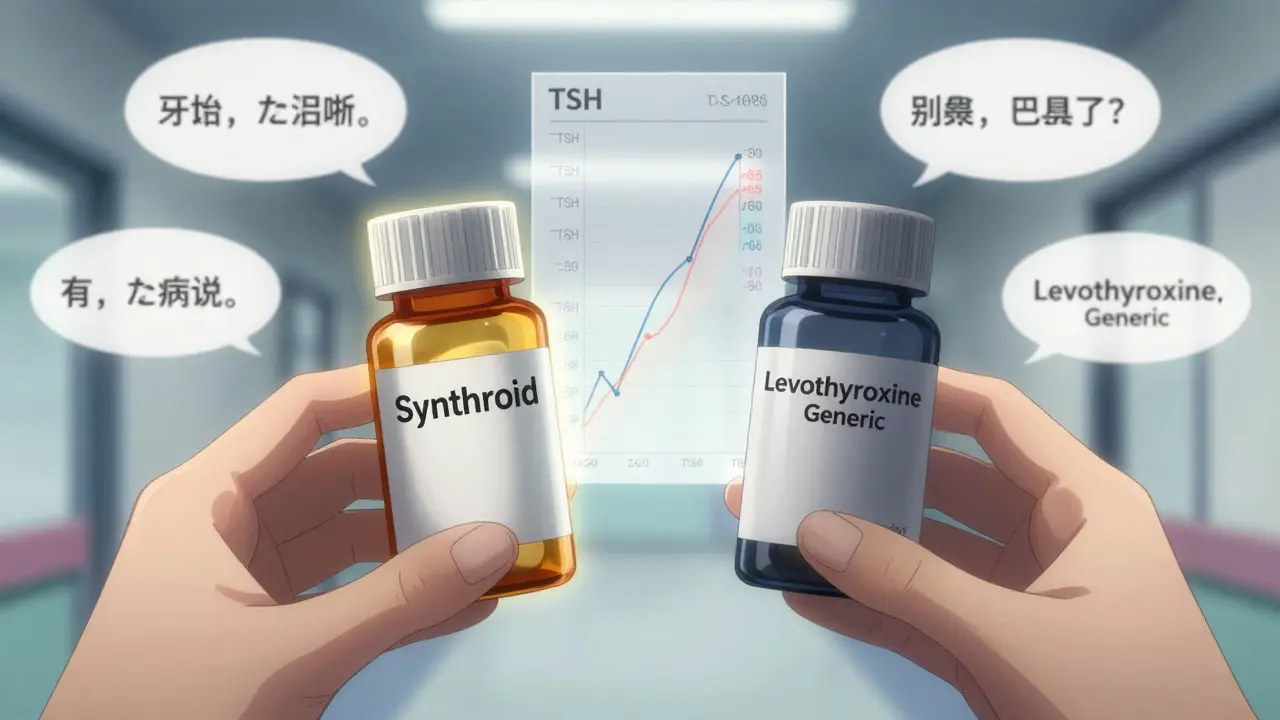
- Your condition worsened-like unstable INR levels on warfarin, new seizures on levetiracetam, or worsening hypothyroid symptoms on levothyroxine.
- Your doctor noticed lab values drifting out of range despite no dosage changes.
- You’ve tried multiple generic versions and had inconsistent results.
The FDA says generics must be within 80%-125% of the brand’s absorption rate. That sounds tight, but for drugs with a narrow therapeutic index-like warfarin, thyroid meds, epilepsy drugs, or immunosuppressants-even small shifts can mean the difference between control and crisis. A 2022 study in JAMA Internal Medicine found that 14.3% of medication-related adverse events were linked to switching between generics and brands, especially when done without oversight.
What’s Really Different Between Brand and Generic?
Both have the same active ingredient. That’s required by law. But here’s what’s not the same:
- Inactive ingredients: Dyes (like FD&C Red #40), preservatives, fillers (lactose, cornstarch), and coatings can trigger allergies or digestive issues. One patient on Reddit reported chronic hives from a generic levothyroxine that vanished the day they switched back to Synthroid.
- Release profiles: Some generics use different manufacturing methods. A delayed-release tablet might dissolve faster or slower than the brand, affecting how much drug enters your bloodstream at once.
- Batch consistency: Brand manufacturers rarely change their formula. Generic makers switch suppliers often. One batch might work perfectly; the next might not.
- Stability: Some generics degrade faster in heat or humidity. In Durban’s climate, this matters more than you think.
That’s why the FDA warns that switching back and forth between brands and generics-especially for narrow therapeutic index drugs-can lead to loss of efficacy or unexpected side effects.
How to Legally and Safely Switch Back
You can’t just walk into a pharmacy and demand the brand. Here’s the real process:
- See your doctor. Don’t self-decide. Bring lab results, symptom logs, and dates of when you started the generic. Say: “I’ve had three different generic versions, and each time my [condition] got worse.”
- Get a written prescription that says ‘Dispense as Written’ (DAW-1). This code tells the pharmacy: “Do not substitute.” Many EHR systems now have a checkbox labeled ‘Brand Medically Necessary’-your doctor must select it.
- Include specific brand name. Don’t write ‘levothyroxine.’ Write ‘Synthroid 50 mcg.’ If you’re on warfarin, write ‘Coumadin.’ Generic names are too vague.
- Provide documentation. Your doctor should complete a CMS Form 1490S (or equivalent) with clinical justification: e.g., ‘Patient developed severe tremors and palpitations after switching to generic levetiracetam. INR fluctuated between 2.1 and 4.8 despite stable dose. Switched back to brand; symptoms resolved within 72 hours.’
- Call your pharmacy ahead. Some pharmacists still don’t recognize DAW-1 codes. Call and say: “I have a prescription with DAW-1. I need the brand name, not a generic.”
- Prepare for insurance battles. Most plans require prior authorization for brand drugs when a generic exists. Your doctor’s office must submit clinical evidence. If denied, appeal immediately. According to the AMA, 63.7% of appeals succeed with proper documentation.
- Follow up within 7-10 days. Recheck labs, symptoms, and side effects. If you’re on thyroid meds, get TSH levels. If on warfarin, get INR. Don’t assume it’s working just because you’re on the brand.
Insurance and Cost Realities
Brand drugs cost 3 to 5 times more than generics. In 2023, the average monthly cost for a brand-name cardiovascular drug was $450.72. The generic? $112.45. Medicare Part D plans deny 68% of brand requests when a generic is available. Blue Cross Blue Shield denied 82% of such requests in user-reported cases.
But here’s the catch: if your doctor properly documents medical necessity, many insurers will cover it. One patient in a Drugs.com review said: “My endocrinologist wrote ‘medically necessary’ on my Synthroid script. Insurance approved it the same day.”
Some states require pharmacists to notify your doctor if you have a bad reaction to a generic. In 17 U.S. states, this is mandatory. South Africa doesn’t have this rule yet, but the same principle applies: if you react badly, speak up.
When You Should NOT Switch Back
Not everyone benefits. The American Academy of Neurology and the American Pharmacists Association warn against switching back for antiepileptic drugs. A 2022 study found a 27% higher rate of breakthrough seizures in patients who switched between different generic or brand versions. The same caution applies to transplant patients on tacrolimus or cyclosporine.
And if your only reason is “I prefer the brand” or “I think it works better”-you’re likely not medically justified. Dr. Jerry Avorn from Brigham and Women’s Hospital says 99.7% of generic switches are fine. Many requests to switch back are driven by perception, not science.
What to Do If You’re Denied
If your insurance denies coverage:
- Ask your doctor to submit a letter of medical necessity with lab results, prior treatment history, and side effect timelines.
- Appeal in writing. Most insurers have a 30-day appeal window.
- Check if the brand offers a patient assistance program. Many manufacturers (like AbbVie for Synthroid) have discounts or free samples.
- Ask your pharmacist if there’s an authorized generic-a brand-made generic sold under a different label. It’s identical to the brand but priced lower.
Final Advice
Switching back isn’t about brand loyalty. It’s about safety. If your body reacts badly to a generic, it’s not ‘all in your head.’ It’s chemistry. The FDA, AMA, and pharmacists agree: when a patient has documented adverse effects or therapeutic failure, switching back to the brand is not just acceptable-it’s necessary.
But don’t do it alone. Get your doctor involved. Document everything. Fight the insurance if you have to. And remember: your health isn’t a cost-cutting metric. It’s your life.
Can I just ask my pharmacist to give me the brand instead of the generic?
No. Pharmacists are legally allowed to substitute a generic unless the prescription says ‘Dispense as Written’ (DAW-1) or ‘Brand Medically Necessary.’ Even if you ask, they’ll fill the generic unless your doctor has specifically required the brand in writing.
Are brand-name drugs more effective than generics?
For most people, no. The active ingredient is identical, and bioequivalence standards ensure similar absorption. But for patients with narrow therapeutic index conditions-like thyroid disease, epilepsy, or blood thinners-small differences in inactive ingredients can lead to clinical instability. In those cases, the brand may be more reliable.
How long does it take for insurance to approve a brand-name drug?
It varies. Some approvals happen in 24 hours. Others take 7-14 days. Medicare Part D beneficiaries reported an average of 14.3 days for prior authorization in 2023. If you’re denied, you can appeal-and 63.7% of appeals succeed with proper documentation.
What if I switch back and still have side effects?
Contact your doctor immediately. It’s possible the brand you received is from a different manufacturer than before, or there’s another issue. Your doctor may need to order therapeutic drug monitoring-like checking TSH, INR, or drug blood levels-to confirm you’re getting the right dose.
Can I switch back if I’m on Medicare?
Yes, but only if your doctor documents medical necessity. Medicare Part D requires prior authorization for most brand drugs when a generic exists. Starting in 2024, a new ‘Medically Necessary Brand Exception’ pathway will guarantee 72-hour processing for certain conditions, including epilepsy, thyroid disorders, and transplant medications.

