More than one in three adults over 60 are taking five or more prescription drugs at the same time. That’s not just common-it’s dangerous. Every pill you take can clash with another, turning a treatment into a threat. A missed dose, a wrong time, or even a common supplement like garlic or fish oil can trigger a reaction that lands you in the hospital. The good news? You don’t have to manage this chaos alone. With a few clear steps, you can cut down the risk of dangerous drug conflicts and take back control of your health.
Keep a Complete, Updated Medication List
Start with the most basic but most overlooked step: write down every single thing you take. Not just your prescriptions. Include over-the-counter painkillers, vitamins, herbal supplements, and even antacids. Many people forget these, but they’re often the hidden cause of problems. For example, taking ibuprofen with blood pressure meds can spike your blood pressure or damage your kidneys. A 2023 study found that 82% of dangerous interactions happen because patients didn’t tell their doctor they were taking something they thought was harmless. Your list needs details. Don’t just write "Lisinopril." Write: Lisinopril 10mg, taken once daily in the morning, for high blood pressure. Include the reason you’re taking it. Note if you’re supposed to take it with food or on an empty stomach. Add special warnings, like "avoid grapefruit" or "take two hours apart from calcium." This isn’t busywork-it’s your safety net. Keep this list in your wallet, on your phone, and share it with every provider you see-even the dentist.Use One Pharmacy for Everything
Switching between pharmacies might seem convenient, but it’s a major risk. If you get your blood pressure meds at one store, your diabetes pills at another, and your painkillers at a third, no single pharmacist has the full picture. A 2023 Health Affairs study showed that when prescriptions are split across multiple pharmacies, pharmacists miss dangerous interactions 53% of the time. That’s more than half the time. Stick with one pharmacy. Most community pharmacies now offer free medication reviews. When you pick up your prescriptions, ask the pharmacist: "Can you check all my meds together for possible conflicts?" They’ll compare everything you’re taking-prescriptions, OTCs, supplements-and flag anything risky. In fact, pharmacies that run full medication therapy management (MTM) programs reduce medication-related problems by 37%, according to Humana’s 2023 data. It takes 20-25 minutes, and it’s free if you’re on Medicare Part D.Try Medication Synchronization
Imagine getting all your monthly meds on the same day-no more juggling different refill dates. That’s medication synchronization. It’s not just about convenience; it’s about safety. When your refills are aligned, you’re less likely to miss a dose or run out unexpectedly. The American Society of Health-System Pharmacists defines it as aligning your maintenance meds to one pickup date each month. Here’s how it works: Your pharmacy identifies your maintenance prescriptions (meds you take daily), separates them from as-needed ones (like pain relievers), and then schedules all your refills for the same day. You might need to fill one or two meds early to get everything synced up, but after that, it’s smooth sailing. Studies show this reduces missed doses by 31% and cuts emergency visits by 22%. Most community pharmacies offer it now-ask if yours does.Use a Pill Organizer-But Choose the Right One
A simple plastic box with compartments for each day of the week is better than nothing. But if you’re taking meds at different times of day, you need more. Look for a 7-day organizer with AM and PM slots. Fill it once a week, preferably on Sunday evening while watching TV. That routine helps you remember. A 2023 University of Michigan study found that patients who filled their organizers during a consistent daily activity improved adherence by 33%. If you struggle with remembering when to take pills, consider a smart organizer with alarms. Devices like Hero Health cost around $899, but they beep, flash, and even text a loved one if you miss a dose. They’re not for everyone, but if you’ve had a close call before, they’re worth it. For most people, though, a basic two-compartment organizer does the job. Just make sure you refill it weekly and never skip.
Know the High-Risk Combinations
Some drug combos are so dangerous they’re on official warning lists. The American Geriatrics Society’s 2023 Updated Beers Criteria lists 30 combinations to avoid in older adults. One of the most common? Taking NSAIDs like ibuprofen or naproxen with blood thinners like warfarin. This combo can cause stomach bleeding or kidney failure. Another is mixing certain antidepressants with migraine meds-this can trigger serotonin syndrome, a rare but life-threatening condition. Also watch for interactions with supplements. St. John’s Wort, a popular herb for mood, can make blood pressure meds, birth control, and even some cancer drugs stop working. Garlic and ginkgo can thin your blood, which is risky if you’re on aspirin or clopidogrel. Always ask your pharmacist before starting anything new-even if it’s labeled "natural."Ask About Deprescribing
Just because a drug was prescribed once doesn’t mean you need it forever. Many older adults take medications they no longer need because no one ever reviewed them. This is called polypharmacy creep. The American Geriatrics Society, the American Society of Health-System Pharmacists, and the American Psychiatric Association all agree: regularly review what you’re taking-and stop what you don’t need. Ask your doctor: "Is there a medication I can stop or lower?" For example, if your blood pressure has improved with diet and exercise, you might not need the full dose anymore. If you’re taking a sleep aid you’ve used for three years, it might be doing more harm than good. Deprescribing isn’t about cutting corners-it’s about simplifying your regimen to reduce risk. One 2023 study found that patients who worked with a pharmacist to reduce unnecessary meds had 41% fewer side effects.Use Digital Tools Wisely
Apps like Medisafe and MyMeds can send reminders, track refills, and alert you to interactions. In a 12-month trial published in JAMA Internal Medicine, users of these apps had 28% higher adherence than those using paper logs. But here’s the catch: 62% of adults over 75 don’t use smartphones regularly. If you’re not comfortable with tech, don’t force it. A paper list and a pill box work just as well. If you do use an app, make sure it lets you enter all your meds-including supplements. And never rely on it alone. Always double-check with your pharmacist. Apps can miss interactions that a human pharmacist catches.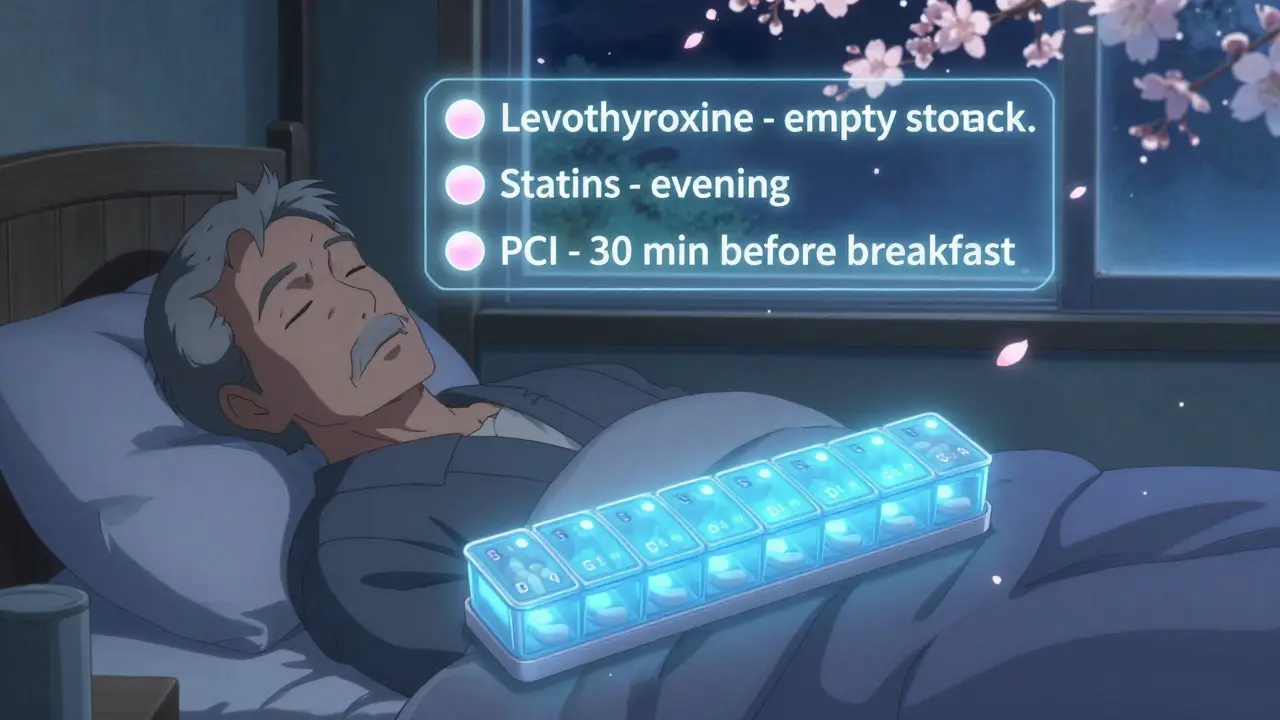
Timing Matters More Than You Think
It’s not just what you take-it’s when. Some meds need space between them. For example, thyroid medication like levothyroxine should be taken on an empty stomach, at least 2 hours before or after calcium, iron, or antacids. If you take them together, your body won’t absorb the thyroid drug properly. Proton pump inhibitors (PPIs) like omeprazole work best when taken 30 minutes before breakfast. If you take them after eating, they won’t reduce acid as well. Blood pressure meds like ACE inhibitors are often more effective when taken at night. And statins for cholesterol work best when taken in the evening, because your liver makes most cholesterol at night. Write down these timing rules on your medication list. Set alarms if needed. Small changes in timing can make a big difference in how well your meds work-and how safe they are.What to Do If You Notice Side Effects
Drowsiness, dizziness, dry mouth, upset stomach, confusion, or unexplained bruising aren’t just annoyances-they’re red flags. A 2023 Healthline review by pharmacist Ami Patel found that 7 out of 10 patients ignore these symptoms, thinking they’re "just getting older." But they’re often signs of drug interactions. If you notice something new, write it down: what you felt, when it started, what meds you took that day. Then call your pharmacist or doctor. Don’t wait. A simple change-like switching a medication or adjusting the dose-can fix it. The sooner you speak up, the less likely you are to end up in the ER.Final Check: Your Personal Medication Plan
Here’s your quick action list:- Make a full list of every pill, supplement, and OTC drug you take-include doses and reasons.
- Use one pharmacy for all your prescriptions.
- Ask your pharmacist for a free medication review.
- Sign up for medication synchronization if available.
- Use a 7-day AM/PM pill organizer and fill it every Sunday.
- Review your list every 3 months-ask if anything can be stopped.
- Know the timing rules for your key meds.
- Report any new side effects immediately.
Managing multiple prescriptions isn’t about being perfect. It’s about being consistent. One small step at a time reduces risk. And over time, that adds up to fewer hospital visits, fewer side effects, and more energy to live your life.
Can I just stop a medication if I think it’s not helping?
No. Never stop a prescription on your own, even if you feel fine. Some medications, like blood pressure or antidepressant drugs, can cause serious withdrawal effects if stopped suddenly. Always talk to your doctor or pharmacist first. They can help you safely reduce or switch a drug if needed.
Are herbal supplements safe to take with my prescriptions?
Not always. Many supplements interact with medications. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can increase bleeding risk if you’re on aspirin or warfarin. Even vitamin K can interfere with blood thinners. Always tell your pharmacist about every supplement you take-even if you think it’s harmless.
Why does my pharmacist ask so many questions when I pick up my meds?
They’re not being nosy-they’re protecting you. Pharmacists are trained to spot drug interactions, duplicate prescriptions, and dosage errors. When they ask about other meds, supplements, or new symptoms, they’re checking for hidden risks. This is especially important if you see multiple doctors. Their job is to catch what others might miss.
Is medication synchronization only for seniors?
No. While it’s most common for older adults on multiple meds, anyone taking three or more maintenance medications can benefit. If you’re managing diabetes, high blood pressure, and cholesterol, or if you take daily pills for asthma, thyroid, or depression, syncing your refills can simplify your routine and reduce missed doses.
How often should I get a medication review?
At least once a year, or anytime you see a new doctor, start a new medication, or notice new side effects. If you’re on eight or more meds and have Medicare Part D, you’re eligible for a free medication therapy management (MTM) session every year. Don’t wait for them to call-ask for it.


Lance Long
January 29, 2026 AT 12:04This hit home hard. My dad took 12 pills a day and never told his cardiologist about the fish oil and garlic supplements he swore were 'just for his heart.' One day he ended up in the ER with internal bleeding. Turned out the combo was cooking his platelets. Now he uses a pill organizer, one pharmacy, and actually writes everything down. I wish we’d known this sooner.
It’s not about being perfect-it’s about being consistent. One small step at a time really does save lives.
Jeffrey Carroll
January 31, 2026 AT 02:18The emphasis on medication synchronization is both practical and underappreciated. Aligning refill dates not only reduces cognitive load but also mitigates the risk of therapeutic gaps. Pharmacists are uniquely positioned to facilitate this process, and their role in polypharmacy management should be formally recognized within primary care models.
Mel MJPS
January 31, 2026 AT 16:31I love how you included the dentist! My mom forgot to tell hers she was on blood thinners-and got a tooth pulled without a consult. Two days later she was in the hospital. Now we make sure every provider gets the list, even the acupuncturist. It’s weird, but it works.
Also, the AM/PM organizer? Game changer. Sunday night with Netflix = no more midnight panic about whether I took my pill.
Ambrose Curtis
February 1, 2026 AT 22:59yo i been usin a smart pill box for 8 months now and it changed my life. Hero Health thing? yeah it’s pricey but my wife gets texts if i miss a dose and she calls me like a mom. i used to forget my blood pressure meds all the time. now i’m not in the hospital. worth every penny.
also st john’s wort? big no. i tried it for ‘anxiety’ and my blood pressure went nuts. pharmacist saved me. always ask em. they’re the real MVPs.
Linda O'neil
February 2, 2026 AT 02:52You’re not alone in this. I used to feel overwhelmed until I started doing my med list every Sunday with my mom. We’d sit at the kitchen table, write everything down, and call her pharmacist together. Now she’s down from 11 meds to 6 after a deprescribing session. She says she feels like she got her energy back.
It’s not about taking fewer pills-it’s about taking the right ones. And you deserve to feel good, not just survive.
doug b
February 2, 2026 AT 03:31One pharmacy. Always. I used to split my meds between CVS and Walgreens because one had cheaper copays. Then I got dizzy and almost passed out. Turned out the two meds were canceling each other out. My pharmacist caught it because she had the full list. Don’t be cheap with your health. It’s not worth it.
And yes, timing matters. I took my thyroid med after breakfast for a year. My TSH was through the roof. Switched to empty stomach? Normal in 6 weeks. Simple fix. Dumb mistake.
Katie Mccreary
February 3, 2026 AT 11:17Wow. So many people are just winging it. This isn’t ‘health advice’-it’s basic survival. If you can’t manage 10 pills, maybe you shouldn’t be on that many. Why do doctors keep prescribing like it’s a buffet?
Also, ‘natural’ doesn’t mean safe. St. John’s Wort is basically a chemical weapon with a yoga vibe.
Kevin Kennett
February 3, 2026 AT 13:27My uncle was on 14 meds. He thought he was being responsible. Turns out half of them were for side effects from the other half. We sat down with his pharmacist, went through every pill, and cut 5. He went from barely walking to gardening again in two months.
Deprescribing isn’t quitting-it’s reclaiming. And if you’re scared to ask your doctor, just say: ‘I want to live better, not just live longer.’ They’ll get it.