When you’re living with end-stage renal disease (ESRD), dialysis isn’t just a medical procedure-it’s a lifestyle. For many, the idea of spending four hours, three times a week, stuck in a clinic chair, surrounded by machines and strangers, becomes unbearable. That’s where home hemodialysis comes in. It’s not a futuristic fantasy. It’s a real, proven option that’s helping thousands of people reclaim their time, energy, and control over their health. But it’s not as simple as plugging in a machine and pressing start. Getting it right means understanding the schedules, committing to serious training, and knowing what outcomes you can realistically expect.
What Home Hemodialysis Actually Looks Like
Home hemodialysis means doing your dialysis treatments in your own living room, bedroom, or even while you sleep. Unlike in-center dialysis, where you’re on someone else’s clock, you decide when to start, how long to go, and how often. There are three main types of schedules, each with different effects on your body and daily life.Conventional home hemodialysis follows the same rhythm as center-based treatment: three times a week, three to four hours each session. The big difference? You can do it at 7 a.m. before work, at 10 p.m. after the kids are asleep, or on a weekend when you’re not rushed. It’s the same amount of dialysis, just more convenient.
Short daily home hemodialysis changes the game. You do five to seven sessions a week, each lasting two to three hours. This means less fluid and toxin buildup between treatments. Patients often report feeling more alert, having better blood pressure control, and needing fewer blood pressure medications. A 2021 study in the Clinical Journal of the American Society of Nephrology found these patients had a 28% lower risk of dying compared to those on conventional in-center dialysis.
Nocturnal home hemodialysis happens while you sleep. You connect to the machine at night and let it run for six to ten hours, three to seven nights a week. This slow, gentle process removes waste and fluid more completely. Studies show it cuts serum phosphate levels by 42% compared to standard dialysis, meaning you can cut back on phosphate binder pills-sometimes by more than three a day. Many patients say they wake up feeling like they’ve had a full night’s rest, not just a dialysis session.
Training Isn’t a One-Week Course-It’s a Commitment
You can’t just watch a YouTube video and start dialyzing at home. Training is mandatory, intense, and personalized. Most programs take between three and eight weeks, though some patients finish in as little as two weeks if they’ve already practiced self-needling during in-center treatments.Training covers more than just how to hook up the machine. You’ll learn:
- How to clean and set up your treatment space
- How to care for your vascular access (fistula or graft) and perform needle insertion
- How to calculate your fluid removal goal based on weight gain
- How to operate and troubleshoot the dialysis machine
- How to store and order supplies without running out
- How to monitor your blood pressure before, during, and after treatment
- How to recognize and respond to alarms, low blood pressure, or bleeding
- How to keep accurate treatment logs for your care team
You’ll also need to pass both written and hands-on tests under supervision. Most programs require you to complete at least 20 to 30 supervised treatments before you’re cleared to go solo. And even then, you’re not alone.
You Need a Care Partner-And That’s Non-Negotiable
Here’s the hard truth: unless you’re one of the rare exceptions with special equipment and approval, you cannot do home hemodialysis alone. Every major health authority-Maryland Department of Health, DaVita, Fresenius-requires a trained care partner to be present during every session.Your care partner isn’t just a helper. They’re your safety net. They need to know how to:
- Insert needles if you can’t
- Stop the machine in an emergency
- Handle a blood leak or air bubble
- Call for help if you pass out or feel dizzy
This requirement is a major barrier. About 30% of people who want home dialysis don’t have someone willing or able to be their partner. Spouses, adult children, or close friends often step up-but it changes relationships. A 2022 Reddit survey of 85 home dialysis users found 41% reported strain in their partnership because of the constant responsibility and stress.
Some newer portable machines, like the NxStage System One, allow for solo treatment under strict conditions. But even then, you need to be approved by your nephrologist and trained in advanced emergency protocols. For most people, the care partner isn’t optional-it’s essential.

What Your Home Needs to Support Dialysis
You don’t need a medical lab in your basement, but you do need a dedicated space. Most machines require a 6-foot by 6-foot area with:- A stable surface for the machine
- A nearby drain for waste fluid
- A clean water line with 40-80 psi pressure
- A dedicated 120-volt, 20-amp electrical circuit
Water quality is critical. Your system must include a reverse osmosis (RO) unit that filters out chemicals, bacteria, and minerals. Monthly water and dialysate cultures are required, and you must keep logs of chlorine levels and disinfection cycles. If your water has high chlorine or chloramine, you’ll need a pre-filter.
Supplies take up space too. You’ll store bags of dialysate, needles, tubing, alcohol wipes, and bandages. Most patients keep a small closet or cabinet just for dialysis supplies. You’ll also need to order supplies monthly-miss a delivery, and you miss a treatment.
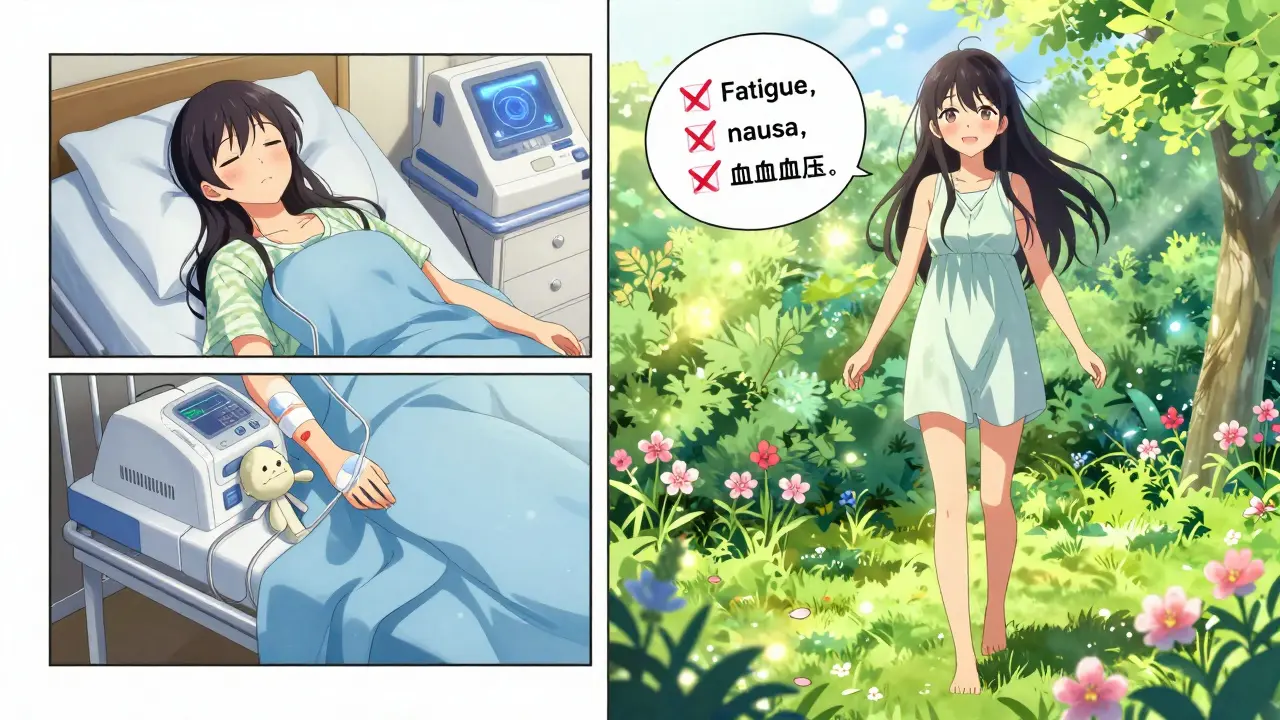
Real Outcomes: Better Health, Better Life
The data doesn’t lie. Home hemodialysis isn’t just more convenient-it’s more effective.A 2019 review in the American Journal of Kidney Diseases found home dialysis patients scored 37% higher on quality-of-life measures than those in centers. They reported more energy, less nausea, and better sleep. A 2020 U.S. Renal Data System report showed home hemodialysis patients had a 15-20% lower risk of death compared to those on in-center dialysis.
But the biggest gains come with frequency. Nocturnal dialysis patients often stop needing phosphate binders entirely. Short daily dialysis patients see fewer hospitalizations for heart failure. One patient in Pittsburgh told his nephrologist he hadn’t been to the ER in two years-something he hadn’t experienced since before he started dialysis.
Still, it’s not perfect. Machine alarms go off at 3 a.m. Supplies arrive damaged. You forget to log a treatment. You panic when the blood pressure drops. A 2023 forum thread on the American Association of Kidney Patients site had 142 responses. Eighty-seven percent said their quality of life improved. Sixty-three percent said they still felt anxious about handling emergencies.
Why More People Aren’t Doing It
If home hemodialysis is better, why is it still only used by about 12% of U.S. dialysis patients?First, access. Only 12% of dialysis centers in the U.S. offer training programs. If you live in a rural area, you might have to drive hours just to start the process.
Second, training capacity. A 2022 survey found 71% of nephrologists say their clinics don’t have enough staff to train more patients. Training takes time-four to six weeks of daily sessions with nurses and educators. Insurance doesn’t always cover the full cost of that staff time.
Third, mindset. Many doctors still assume patients aren’t capable. But the truth is, patients who are motivated, have support, and are given the right training succeed. The University of Washington Medical Center cut training time to 3-4 weeks using virtual reality simulators for needle practice. Their patient competency rate jumped from 78% to 92%.
What’s Changing in 2026
The dialysis landscape is shifting. The 2021 Advancing American Kidney Health initiative aimed for 80% of new ESRD patients to start on home dialysis or transplantation by 2025. That goal won’t be met-but progress is happening.New portable machines like the NxStage System One and the WavelinQ endoAVF system are making home dialysis easier to travel with and easier to set up. Medicare’s reimbursement rules are changing too. Starting in 2025, payments will be tied to patient outcomes-not just how many treatments you do. That means clinics will have a financial incentive to push home dialysis, because patients on home dialysis have fewer complications and hospital stays.
For patients, this means more support, better training tools, and more options. But the core truth hasn’t changed: home hemodialysis works best when you’re ready-not just physically, but mentally and emotionally. You need to want it. You need to be prepared. And you need someone who’s ready to stand by you, even when the machine beeps at 2 a.m.
Can I do home hemodialysis alone?
Almost always, no. Most health guidelines require a trained care partner to be present during every treatment. Solo home hemodialysis is only allowed with special equipment, advanced training, and approval from your nephrologist. Even then, it’s rare and comes with strict safety rules. The risk of being alone during a medical emergency is too high for most programs to allow it.
How long does home hemodialysis training take?
Training usually lasts between three and eight weeks, depending on your learning pace, the type of machine, and whether you’ve practiced self-needling before. Most programs require 20-30 supervised sessions before you’re cleared. Some patients finish in as little as two weeks if they’re already familiar with the process. The key is not time-it’s competency. You must pass both written and practical exams before going home.
Is home hemodialysis cheaper than in-center dialysis?
Medicare pays the same amount whether you do dialysis at home or in a center. But for patients, home dialysis can save money indirectly. You’ll spend less on transportation, meals outside the home, and time off work. Many patients report saving 10 or more hours per week just by avoiding clinic trips. There are also fewer hospital visits, which reduces out-of-pocket costs for emergencies.
What if my care partner can’t continue?
If your care partner becomes unavailable-due to illness, relocation, or burnout-you must stop home dialysis until you find a replacement. Your dialysis center can help you identify a new partner or transition back to in-center treatment. Some patients train a second person as a backup. It’s important to have a plan before you start, because you can’t do it alone without special approval.
Can I travel with a home hemodialysis machine?
It depends on the machine. Standard home hemodialysis machines are not portable-you’ll need to schedule treatments at a clinic when you travel. But portable systems like the NxStage System One are designed for travel. You can take them on planes, in cars, or to vacation homes. You’ll still need to plan ahead: arrange for water, power, and dialysate delivery at your destination. Some patients ship supplies ahead or use local dialysis centers for backup.
Does home hemodialysis improve survival?
Yes, studies consistently show better survival rates for home hemodialysis patients compared to those on in-center dialysis. The U.S. Renal Data System found a 15-20% lower mortality rate for home patients. The biggest benefit comes with frequent or long treatments-like short daily or nocturnal dialysis. These schedules remove toxins more completely and reduce stress on the heart, leading to fewer hospitalizations and longer life.
What are the most common problems with home hemodialysis?
The most frequent complaints are machine alarms (67%), managing supplies (58%), and dependency on a care partner (52%). Many patients also struggle with anxiety during the first few months, especially when handling needles or responding to emergencies. Some report feeling isolated or overwhelmed. But these issues usually improve with time, better training, and support from patient communities.
Who is not a good candidate for home hemodialysis?
People with severe cognitive impairment, uncontrolled mental health conditions, or physical limitations that prevent them from handling equipment are not good candidates. Those without a reliable care partner, or who live in homes without proper plumbing or electrical setup, also face major barriers. If you’re not motivated to learn or manage your own care, home dialysis will be more stressful than helpful.
Next Steps: Is Home Hemodialysis Right for You?
If you’re considering home hemodialysis, start by talking to your nephrologist. Ask if your center offers training. Ask how many patients they’ve trained in the past year. Ask about their success rates and how they handle emergencies.Visit Home Dialysis Central or the National Kidney Foundation’s website to read patient stories. Talk to someone who’s been doing it for a year. Ask them what they wish they’d known.
This isn’t a decision to rush. But it’s one worth exploring. For many, home hemodialysis isn’t just better treatment-it’s the difference between surviving and living.


Kelly Beck
January 4, 2026 AT 21:50Just finished my 6-month mark on nocturnal home dialysis and I’m still in awe. I used to wake up exhausted, now I wake up like I actually slept. No more 3 p.m. crashes, my BP meds are down to half, and I’ve started hiking again. The first month was brutal-needle anxiety, machine alarms at 2 a.m., my husband nearly quit-but we got through it. If you’re on the fence, just try one short daily session at the clinic first. You’ll feel the difference in your bones. This isn’t just treatment-it’s a second chance at life. 🙌
Wesley Pereira
January 5, 2026 AT 03:14So let me get this straight-you’re telling me we’re now pushing home dialysis because it’s ‘better’ but still require a live-in nurse? Classic. The system gives you the option, then makes it so logistically impossible you’re forced back to the clinic. They call it ‘empowerment’ but it’s just cost-shifting with a smiley face. And don’t even get me started on the ‘care partner’ requirement-like, sure, my wife is amazing, but she’s not a nurse. And now she’s got PTSD from the time I went hypotensive during a storm. Thanks, healthcare industrial complex.
Vinayak Naik
January 6, 2026 AT 16:40Man, I’ve been doing short daily for 2 years. The hardest part? Not the needles. Not the alarms. It’s the grocery list. You gotta track dialysate, needles, wipes, saline, alcohol, tape, gloves, and then the RO unit filters. Miss one delivery? You miss a session. I once had a package stuck in customs for 10 days. I was on IV fluids for 3 days just to survive. But? I went from ‘I can’t walk to the mailbox’ to biking to the coffee shop. Worth every headache. And yes, I still cry when the machine beeps at 3 a.m. But now I laugh while I cry.
Susan Arlene
January 8, 2026 AT 06:19my machine beeped at 3am again. i just stared at the ceiling. didn't move. it stopped. i went back to sleep. this is my life now. no drama. no fanfare. just me, the machine, and the quiet.
Leonard Shit
January 10, 2026 AT 01:52Y’all act like home dialysis is some revolutionary hack. It’s just… medicine. We’ve been doing this since the 80s. The real issue? No one in the system gives a damn about training time or staffing. You’re supposed to be ‘empowered’ but your clinic’s got one nurse for 40 patients. And they wonder why people drop out. Also, ‘care partner’? Yeah, my mom’s 78 and has COPD. She’s my ‘partner’ because I have no other options. That’s not empowerment-that’s guilt wrapped in a brochure.
Pavan Vora
January 11, 2026 AT 07:04As someone from India, I find it fascinating that home hemodialysis is even considered here… in the U.S., where infrastructure is… well, let’s say, inconsistent. In my hometown, we don’t even have reliable electricity, let alone reverse osmosis units. But I’ve seen patients in Pune who do it-on solar-powered machines, with hand-pumped water. They’re not ‘empowered’-they’re survivors. And yet, here in America, we’re debating whether to make it easier? The irony is… profound.
Venkataramanan Viswanathan
January 12, 2026 AT 21:57While the clinical outcomes are statistically compelling, the socio-structural barriers remain grossly under-addressed. The requirement of a trained care partner, while ostensibly a safety protocol, functions as a de facto exclusionary mechanism for those without familial or social support networks. Furthermore, the logistical burden of supply chain management, coupled with inconsistent insurance reimbursement for ancillary equipment, renders this modality inaccessible to a significant proportion of the population. The narrative of patient autonomy is thus, in practice, a privilege.
Ashley S
January 14, 2026 AT 16:54Why are we even talking about this? People are too lazy to go to the clinic. They want to do it at home so they can binge Netflix. Meanwhile, the nurses are overworked, the machines break down, and someone’s gotta clean up the blood spills at 2 a.m. This isn’t freedom-it’s a burden we’re forcing on families. And don’t even get me started on the cost to taxpayers. We should just make clinics better, not turn patients into unpaid technicians.
Tom Swinton
January 14, 2026 AT 19:06I just want to say-thank you to every care partner out there. Seriously. I watched my brother do this for his wife for three years. He never missed a session. He learned how to do needle sticks. He stayed up all night when the alarm went off. He never complained. Not once. And now? She’s running marathons. He’s still tired. He still has nightmares about blood leaks. But he’d do it again. To anyone reading this: if you’re a care partner, you’re a hero. And if you’re thinking about it? You’re braver than you know.
Isaac Jules
January 15, 2026 AT 03:30Home dialysis? More like home disaster. You think you’re in control? Nope. You’re just the guy who gets to clean up the mess when the machine fails, the water’s contaminated, or your partner passes out. And don’t tell me about ‘studies’-I’ve seen the ER logs. The number of cardiac arrests from home dialysis complications? Higher than you think. And now we’re pushing this as a ‘solution’? Wake up. This isn’t innovation-it’s negligence dressed up in a motivational poster.
Joann Absi
January 16, 2026 AT 13:56AMERICA IS THE ONLY COUNTRY THAT THINKS IT’S ‘EMPOWERING’ TO MAKE SICK PEOPLE DO THEIR OWN MEDICAL PROCEDURES WHILE THEIR WIVES CRY IN THE OTHER ROOM. IN JAPAN, THEY HAVE NURSES COME TO YOUR HOUSE. IN CANADA, THEY PAY FOR 24/7 SUPPORT. BUT HERE? WE MAKE YOU BECOME A NURSE OR JUST DIE IN THE LIVING ROOM. THIS ISN’T FREEDOM. THIS IS CRUELTY.
Brian Anaz
January 17, 2026 AT 18:44Home dialysis sounds great until you realize you’re paying $200 a month just for dialysate bags. And don’t get me started on the water filter. RO unit cost $3K. Maintenance? $500/year. Insurance pays for the machine, but not the damn water. So now I’m a water quality technician on top of being a patient. And they wonder why people go back to the clinic? It’s not fear-it’s economics.
Mukesh Pareek
January 18, 2026 AT 16:45The data is clear: nocturnal HD reduces phosphate burden by 42%, as cited in the CJASN meta-analysis. However, the compliance rate for water culture logs remains below 60% in community-based programs, indicating a critical gap in protocol adherence. Furthermore, the absence of standardized competency benchmarks across dialysis centers introduces significant heterogeneity in outcomes. Without mandatory certification for care partners, this modality remains a high-risk, high-reward proposition with unacceptably variable safety profiles.
Indra Triawan
January 20, 2026 AT 01:01Do you ever feel like your body is just… a machine you have to tend to? Like, you’re not a person anymore-you’re a system. A series of tubes, pressures, and filters. I used to dream of the ocean. Now I dream of silence. Not peace. Just… silence. No beeps. No alarms. No one asking if I’m okay. Just me. And the dark. And the machine waiting.
Rachel Wermager
January 20, 2026 AT 22:33Let’s be real-most nephrologists still don’t understand home dialysis. They’ll say ‘it’s an option’ but won’t refer you unless you’re ‘ideal.’ What’s ideal? White, middle-class, married, literate, and with a spouse who can take off work. The system isn’t broken-it’s designed to exclude the vulnerable. And now they’re calling it ‘patient-centered care’? Please. The real innovation isn’t the machine-it’s the fact that some patients are still alive because they refused to accept the status quo.