Dental Anesthetic Safety Calculator
Anesthetic Safety Calculator
Calculate the maximum safe dose of dental local anesthetics based on patient weight and the specific anesthetic agent. Essential for safe administration and avoiding overdose.
When dentists need a painless bite, local anesthesia in dentistry is the practice of numbing specific areas of the mouth so procedures can be performed without pain. From the clumsy ether masks of the 19th century to today’s computer‑controlled delivery systems, the story is full of curious experiments, scientific breakthroughs, and a few dramatic courtroom dramas.
Quick Takeaways
- Ether was the first volatile anesthetic used in dental work (1846).
- Cocaine became the first widely accepted dental anesthetic in the 1880s, despite its toxicity.
- Procaine (Novocain) introduced the era of synthetic, safer agents.
- Lidocaine, discovered in 1948, remains the workhorse of modern dentistry.
- Today’s formulations focus on faster onset, longer duration, and reduced allergic reactions.
Early Experiments: The Ether Age
On October 16, 1846, William Morton is an American dentist who demonstrated the use of ether as a surgical anesthetic at Massachusetts General Hospital. He inhaled ether through a mask while a patient underwent a tooth extraction, and the patient reported no pain. That demonstration sparked worldwide interest, and dentists began to experiment with ether‑filled cups and gauze. The technique was messy, the smell was harsh, and dosage control was a gamble-still, it proved that pain could be blocked.
Cocaine Takes the Stage
In 1884, Carl Koller is an Austrian ophthalmologist who discovered that cocaine could anesthetize the eye and later the oral cavity. Dentists quickly adopted cocaine because it worked quickly and allowed precise numbing of individual teeth. However, the drug’s addictive potential and side‑effects-like elevated heart rate and tissue irritation-soon raised alarms. By the early 1900s, regulations limited its dental use, prompting the search for safer synthetic alternatives.
The Synthetic Revolution: Procaine (Novocain)
German chemist Alfred Einhorn is the inventor of procaine, marketed as Novocain, in 1905. Procaine offered a longer duration and lower toxicity compared to cocaine, though it had a slower onset. Dentists liked the fact that it could be mixed with epinephrine to constrict blood vessels and prolong numbness. The trade‑off was a slight metallic taste and occasional allergic reactions, but overall it marked the beginning of modern dental anesthetic chemistry.
Mid‑Century Milestones: Lidocaine and Beyond
In 1948, Swedish chemist Nils Löfgren is credited with synthesizing lidocaine, a fast‑acting local anesthetic with excellent safety profile. Lidocaine’s rapid onset (1-3 minutes) and moderate duration (30-120 minutes) made it the go‑to choice for most dental procedures. By the 1970s, manufacturers introduced lidocaine with epinephrine and buffered solutions to reduce injection pain.
Another breakthrough came in 1976 with Articaine is a benzocaine derivative that contains a thiophene ring, allowing higher lipid solubility and faster nerve penetration. Articaine’s shorter half‑life means quicker recovery, and many clinicians favor it for deep blocks.
Modern Techniques and Delivery Systems
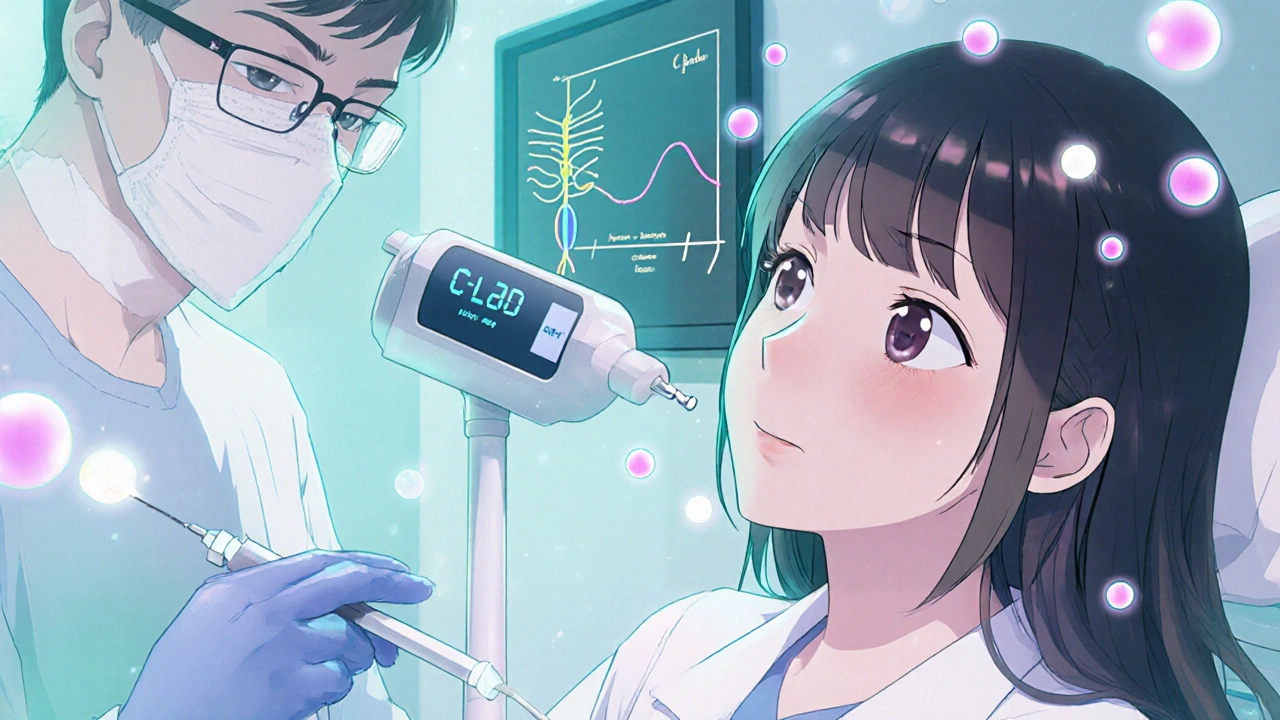
Today's dentists rarely rely on the old ether masks. Instead, they use disposable syringes with fine‑gauge needles and, increasingly, computer‑controlled local anesthetic delivery (C-CLAD) devices that regulate pressure and flow. Topical anesthetic gels (e.g., benzocaine or lidocaine patches) are applied before injections to further reduce needle sting.
Another trend is the use of nitrous oxide is a colorless gas also known as laughing gas, used for its anxiolytic and mild analgesic effects as a sedative adjunct. While not a true local anesthetic, it enhances patient comfort during longer procedures.
Future Directions: Nanocarriers and Liposomal Formulations
Researchers are testing liposomal lidocaine that releases the drug slowly over hours, aiming to reduce postoperative pain without repeat injections. Nanoparticle carriers promise even more precise targeting of nerves, potentially minimizing systemic exposure.
Side‑by‑Side Comparison of Major Dental Anesthetics
| Agent | Year Introduced | Onset (min) | Duration (min) | Max Safe Dose (mg/kg) | Typical Use |
|---|---|---|---|---|---|
| Ether | 1846 | 5-10 | 30-60 | Varies (volatile) | Historical demonstration |
| Cocaine | 1884 | 1-2 | 45-120 | 0.5-1.0 | Early dental blocks |
| Procaine (Novocain) | 1905 | 5-10 | 60-120 | 6-7 | General extractions |
| Lidocaine | 1948 | 1-3 | 30-120 | 4.5-7 | Standard infiltration & block |
| Articaine | 1976 | 1-2 | 20-60 | 6-7 | Deep mandibular blocks |
Common Pitfalls and How to Avoid Them
- Over‑injecting: Always calculate the maximum safe dose based on patient weight.
- Failing to aspirate: Pull back the plunger before injecting to avoid intravascular delivery.
- Ignoring allergies: Ask patients about previous reactions to anesthetics, especially procaine or lidocaine.
- Using stale cartridges: Anesthetic solutions degrade over time; check expiration dates.
Mini FAQ
When was the first local anesthetic used in dentistry?
Ether was first demonstrated for dental extraction by William Morton in 1846, marking the birth of local anesthesia in dentistry.
Why did dentists switch from cocaine to synthetic agents?
Cocaine caused cardiovascular stimulation and had high abuse potential. Synthetic agents like procaine offered lower toxicity and better control over duration.
Is articaine safe for all patients?
Articaine is generally safe, but a small percentage of patients may experience methemoglobinemia, especially with high doses. Screening for enzyme deficiencies is advisable.
How does computer‑controlled delivery improve patient comfort?
C‑CLAD devices regulate injection pressure, preventing the sudden “pressure spike” that triggers pain receptors, resulting in a smoother, less intimidating experience.
What’s the future of dental anesthesia?
Emerging liposomal and nanoparticle formulations aim to extend pain control beyond the procedure, while reducing systemic side effects. Personalized dosing based on genetic markers is also on the horizon.
Understanding the evolution of local anesthesia dentistry not only gives us respect for the pioneers who endured trial‑and‑error, it also shows why modern practice feels so safe and precise. Whether you’re a student, a seasoned dentist, or simply curious, knowing the past helps you appreciate the comfort you experience during a routine filling today.


Sajeev Menon
October 22, 2025 AT 18:00Hey folks, just wanted to add a quick tip for anyone still calculating dosages on the fly – always base the max safe dose on the patient’s weight, not just the surface area of the tooth. It’s a simple step that can prevent a lot of over‑injecting mishaps. Also, never forget to aspirate before you push the plunger; it’s a tiny move that saves you from intravascular delivery. And, uh, keep an eye on the expiration dates of those cartridges – stale solutions can lose potency faster than you think.
Stay safe out there!
Kiara Gerardino
October 26, 2025 AT 04:20The cavalier adoption of cocaine in early dentistry was nothing short of a moral fiasco. Ignoring its addictive potential for the sake of quick numbness reflects a reckless disregard for patient welfare. Modern practitioners should be ashamed of those historical shortcuts and champion safer, ethically vetted agents. Let’s ensure history’s mistakes never repeat under the guise of progress.
Tim Blümel
October 29, 2025 AT 15:40What a fascinating journey from ether to nanocarriers! 🌟 The evolution shows how philosophy meets practice – we constantly question how to balance efficacy with safety. 🤔 Kudos to the pioneers who dared to experiment, and props to today’s researchers pushing the boundaries of targeted delivery. Keep the curiosity alive, and remember: every breakthrough starts with a single, brave idea. 🚀
Emily Collins
November 2, 2025 AT 03:00Your post reads like a nostalgic tour de force.
Sarah Riley
November 5, 2025 AT 14:20From a pharmacodynamic standpoint, the shift toward liposomal lidocaine epitomizes a strategic optimization of therapeutic index, leveraging controlled release kinetics to mitigate systemic exposure.
Tammy Sinz
November 9, 2025 AT 01:40The prospective integration of nanoparticle carriers could revolutionize anesthetic precision, delivering agents directly to nociceptive fibers while preserving adjacent tissue integrity. Such advancements align with patient‑centric care models and merit immediate attention in clinical protocols.
Wade Grindle
November 12, 2025 AT 13:00Interesting read! I’ve seen similar anesthetic trends across Europe and Asia, where adoption of computer‑controlled delivery has noticeably improved patient comfort. It’s great to see the global community converging on best practices.
Jai Reed
November 16, 2025 AT 00:20Dear colleagues, the historical progression of dental local anesthesia underscores a relentless pursuit of safety and efficacy, a principle that must remain paramount in contemporary practice. From the crude ether masks of the mid‑19th century to the sophisticated C‑CLAD devices of today, each innovation reflects a response to the shortcomings of its predecessor. The early reliance on ether, while groundbreaking, suffered from uncontrolled dosage and hazardous flammability, prompting the urgent need for more manageable agents. Cocaine’s introduction provided rapid onset but introduced unacceptable cardiotoxicity and addiction risks, compelling the field to search for synthetic alternatives. Procaine, albeit slower in onset, marked a pivotal shift toward reduced toxicity and the inclusion of epinephrine to prolong anesthesia duration. However, its metallic taste and occasional allergic reactions highlighted the necessity for further refinement. Lidocaine’s advent in 1948 fulfilled many of these criteria, delivering swift onset, moderate duration, and a favorable safety profile, establishing it as the workhorse of modern dentistry. Articaine’s enhanced lipid solubility and abbreviated half‑life have since expanded the clinician’s armamentarium, offering deeper blocks with quicker recovery. Contemporary delivery systems, particularly computer‑controlled devices, address the ergonomic and pain‑related challenges of traditional syringes by modulating pressure and flow, thereby minimizing the infamous “pressure spike” that triggers nociceptor activation. Furthermore, adjunctive modalities such as topical gels and nitrous oxide complement local anesthetics, enhancing patient comfort and reducing anxiety. Looking ahead, the development of liposomal and nanoparticle carriers promises sustained analgesia, potentially obviating the need for repeat injections and reducing systemic exposure. These formulations also open avenues for personalized dosing based on genetic markers, heralding an era of precision anesthesiology. It is incumbent upon practitioners to stay abreast of these advances, critically evaluate emerging evidence, and integrate validated technologies into routine care to uphold the highest standards of patient safety and experience.