Every year, millions of people in the U.S. receive the wrong medication, wrong dose, or a drug that clashes dangerously with what they’re already taking. These aren’t rare accidents-they’re preventable mistakes happening in pharmacies across the country. In fact, a 2023 global review found that dispensing errors occur in about 1.6% of all prescriptions filled. That might sound small, but when you’re talking about hundreds of millions of prescriptions annually, it adds up to millions of patients at risk.
What Are the Most Common Dispensing Errors?
Pharmacists don’t make mistakes because they’re careless. They make them because systems are flawed. The most frequent errors fall into a few clear categories:- Wrong medication: Giving a patient Celebrex instead of Celexa, or Amoxicillin instead of Augmentin. Sound-alike or look-alike names cause nearly 30% of these mix-ups.
- Wrong dose or strength: A 500mg tablet instead of a 250mg, or a 10mg/mL concentration instead of 5mg/mL. This is especially dangerous with drugs like insulin, warfarin, or opioids.
- Wrong dosage form: Giving a patient an extended-release pill when they were prescribed an immediate-release version-or worse, crushing a tablet that shouldn’t be crushed.
- Missing drug interactions: Failing to catch that a patient on blood thinners was just prescribed a new NSAID, or that an antibiotic cancels out the effectiveness of birth control.
- Incorrect duration: Dispensing a 90-day supply when the prescription called for 30 days, or vice versa.
- Expired or improperly stored meds: Medications that degrade because they were kept in heat or humidity, or weren’t rotated properly on the shelf.
According to the Academy of Managed Care Pharmacy, these three types account for 84% of all dispensing errors: incorrect medication/dose/form (32%), miscalculated dose (28%), and missed contraindications (24%).
Why Do These Errors Keep Happening?
It’s easy to blame the pharmacist. But the real problem isn’t people-it’s pressure, poor design, and outdated processes.- Workload overload: Pharmacists in busy community pharmacies may fill 250-300 prescriptions a day. That’s one every 2-3 minutes. When you’re racing, mistakes creep in.
- Handwritten prescriptions: Even in 2025, 43% of errors still come from illegible handwriting. A sloppy “5” looks like a “9.” A slanted “U” looks like a “0.”
- Sound-alike, look-alike drugs: Drugs like Hydralazine and Hydroxyzine, or Premarin and Prempro, are easy to confuse. One wrong pick can cause a stroke or a dangerous allergic reaction.
- Interruptions: A phone call, a customer question, a nurse asking for a refill-all of these break focus. Studies show that if a pharmacist gets interrupted three or more times while filling a prescription, the chance of error jumps by over 12%.
- Missing patient info: No allergy history? No renal function numbers? No list of current meds? That’s not the pharmacist’s fault-it’s a broken system.
And it’s not just community pharmacies. Hospital pharmacies see even more complexity: IV bags mixed wrong, pumps programmed at the wrong rate, antibiotics given too fast. Vancomycin given too quickly can cause “red man syndrome”-a painful, potentially life-threatening flush. That’s not a mistake you want to make.
Which Medications Are Most Often Involved?
Some drugs are just more dangerous when messed up. The most common culprits in serious errors:- Anticoagulants (like warfarin or apixaban): Involved in 31% of serious cases. A tiny dose error can cause internal bleeding.
- Antimicrobials (antibiotics): 28% of errors. Wrong drug or dose can lead to resistant infections or allergic reactions.
- Opioids: 24% of errors. Too much can cause respiratory failure.
- Anticonvulsants and antidepressants: Changes in dose can trigger seizures or suicidal thoughts.
And here’s something chilling: In antibiotic-related errors, 41% happened because the pharmacist didn’t check the patient’s allergy history. Another 29% were because they didn’t cross-check the drug’s ingredients against known allergies. That’s not a lack of skill-it’s a lack of system.

How to Stop These Errors Before They Happen
The good news? We know how to fix this. It’s not about working harder-it’s about working smarter.1. Use Barcode Scanning
Barcodes on medication bottles and patient wristbands are one of the most proven tools. A 2021-2023 survey of 127 hospitals showed that barcode systems cut dispensing errors by 47.3%. Wrong drug? Scanned and flagged. Wrong dose? System blocks it. Wrong patient? It catches that too. One community pharmacist reported catching 12 serious errors in their first month of using barcode scanning.
2. Implement Double Checks for High-Risk Drugs
For insulin, heparin, chemotherapy, and opioids, two trained staff members should verify the medication before it leaves the pharmacy. One pharmacy in Ohio reduced insulin errors by 78% after adopting this rule. It doesn’t slow things down-it prevents disasters.
3. Use Tall Man Lettering
This is simple: write similar-looking drugs in a way that highlights the difference. For example:
- HYDROXYzine vs. HYDRAZIPine
- LEVOTHYROxin vs. LEVOTIroxine
When 214 community pharmacies adopted this, sound-alike errors dropped by 56.8%. It’s a tiny change with a huge impact.
4. Don’t Crush Tablets Unless It’s Safe
Many extended-release or enteric-coated pills should never be crushed. Crushing them can release the full dose at once-dangerous with opioids or blood pressure meds. The ISMP’s “Do Not Crush” list, now used in 89% of long-term care facilities, cut crushing errors by 73%.
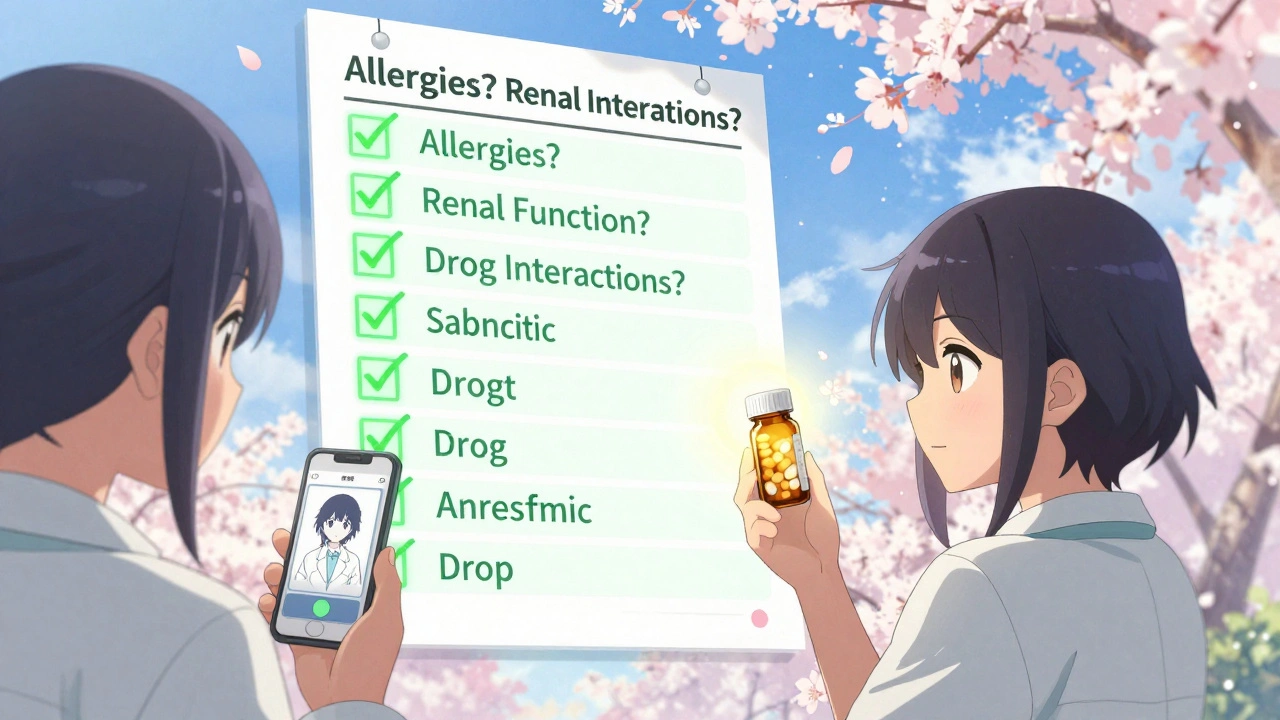
5. Require Full Patient Profiles
Before dispensing, pharmacists should review:
- Current medications (including OTC and supplements)
- Allergies (and the exact reaction)
- Renal and liver function
- Weight (for pediatric and obese patients)
- Pregnancy status
If the system doesn’t show this, the pharmacist should call the prescriber. No exceptions.
6. Use Clinical Decision Support
Computerized systems that flag interactions, duplicate therapies, or incorrect doses are powerful. But they’re not perfect. A 2023 study found that while these systems cut errors by 43%, they also created new problems-like alert fatigue. Too many pop-ups, and staff start ignoring them. The key? Smart alerts. Only trigger warnings for high-risk combinations, not every minor interaction.
What’s Next for Pharmacy Safety?
Technology is advancing fast. AI systems are being tested to predict which prescriptions are most likely to have errors based on historical data, patient history, and prescriber patterns. One hospital system reduced errors by over 52% using AI-assisted checks.Robotic dispensing units are also growing. They can fill hundreds of prescriptions with near-zero human error. But they cost $150,000 to $500,000-and they’re not foolproof. If the robot gets loaded with the wrong bottle, it’ll keep dispensing the wrong drug.
The biggest shift coming? Standardized global reporting. Right now, every country, every hospital, every pharmacy uses different definitions for what counts as an error. That makes it impossible to learn from each other. The WHO and ISMP are launching a unified classification system in early 2025. Once adopted, it could reduce international error rates by up to 35%.
What Patients Can Do
You’re not powerless. You can protect yourself:- Ask: “Is this the same as what I got last time?”
- Check the pill against the label-color, shape, imprint code.
- Ask the pharmacist: “What is this for? What side effects should I watch for?”
- Keep a list of all your meds-including vitamins and herbal supplements-and bring it to every appointment.
- If something looks wrong, speak up. Don’t assume the pharmacist knows better.
Pharmacists are trained to catch errors. But they’re human. Systems are meant to catch what humans miss. When both work together, mistakes drop-not because someone’s perfect, but because the system isn’t relying on perfection.
Frequently Asked Questions
What’s the most common cause of pharmacy dispensing errors?
The most common cause is workload pressure combined with poor system design. Pharmacists are expected to fill hundreds of prescriptions a day with little time for verification. Interruptions, illegible handwriting, and similar-looking drug names compound the problem. It’s rarely about carelessness-it’s about flawed workflows.
Can barcode scanning really prevent most errors?
Yes. Studies show barcode scanning reduces dispensing errors by nearly half. It’s especially effective at catching wrong drugs, wrong doses, and wrong patients. In one hospital, it stopped 12 potentially fatal errors in just the first month of use. It’s not 100% foolproof, but it’s the single most effective tool most pharmacies can implement today.
Why do some medications cause more errors than others?
Drugs with narrow therapeutic indexes-like warfarin, insulin, or digoxin-are dangerous even in small overdoses. Also, drugs with similar names (e.g., hydralazine vs. hydroxyzine) or those commonly misused (opioids, antibiotics) are more likely to be picked by mistake. These are called “high-alert medications,” and they require extra checks.
Do electronic prescriptions reduce errors?
Yes, but not always. E-prescribing cuts errors from handwriting by 90%. However, if the system has poor decision support, it can create new problems-like alert fatigue, where pharmacists start ignoring warnings because there are too many. The best systems combine e-prescribing with smart alerts and require pharmacist confirmation for high-risk matches.
How can I tell if I got the wrong medication?
Compare the pill to the label: check the name, dose, and number of pills. Look up the pill’s imprint code online using a trusted site like Drugs.com. If it doesn’t match, or if the color/shape is different from your last fill, ask the pharmacist to double-check. Don’t take it home if something feels off.
What to Do If You Suspect an Error
If you think you received the wrong medication:- Don’t take it.
- Call the pharmacy immediately and ask to speak to the pharmacist.
- Keep the original packaging and label.
- If you’ve already taken it and feel unwell, call 911 or go to the ER.
- Report the error to your state’s pharmacy board or the FDA’s MedWatch program.
Pharmacy errors are preventable. But they won’t disappear until we stop blaming individuals and start fixing systems. The tools are here. The data is clear. What’s missing is the will to use them-consistently, everywhere.


val kendra
December 5, 2025 AT 09:10Libby Rees
December 6, 2025 AT 07:37Ben Choy
December 8, 2025 AT 05:35Karl Barrett
December 9, 2025 AT 23:31Scott van Haastrecht
December 11, 2025 AT 15:07Jenny Rogers
December 12, 2025 AT 20:27Emmanuel Peter
December 13, 2025 AT 03:30Heidi Thomas
December 14, 2025 AT 17:06Isabelle Bujold
December 15, 2025 AT 07:26Rudy Van den Boogaert
December 15, 2025 AT 09:59Jordan Wall
December 16, 2025 AT 15:30Shofner Lehto
December 18, 2025 AT 02:43John Filby
December 19, 2025 AT 10:28Elizabeth Crutchfield
December 19, 2025 AT 22:45