You rarely hear stories of blood clots making the evening news, but here’s a number to remember: pregnant women are about five times more likely to develop a blood clot than those who aren’t expecting. Blood that clots too easily might sound like the bad guy from a medical thriller—a silent threat that rarely strikes, but when it does, the consequences can turn serious fast. Most people wouldn’t expect growing a baby to increase your risk of deep vein thrombosis (DVT) or pulmonary embolism, but your body ramps up blood-clotting factors during pregnancy for a reason, even if it isn’t always on your side. If you want a healthy ride from bump to baby, understanding the risks and how to spot trouble is half the battle.
Why Pregnancy Raises the Risk of Blood Clots
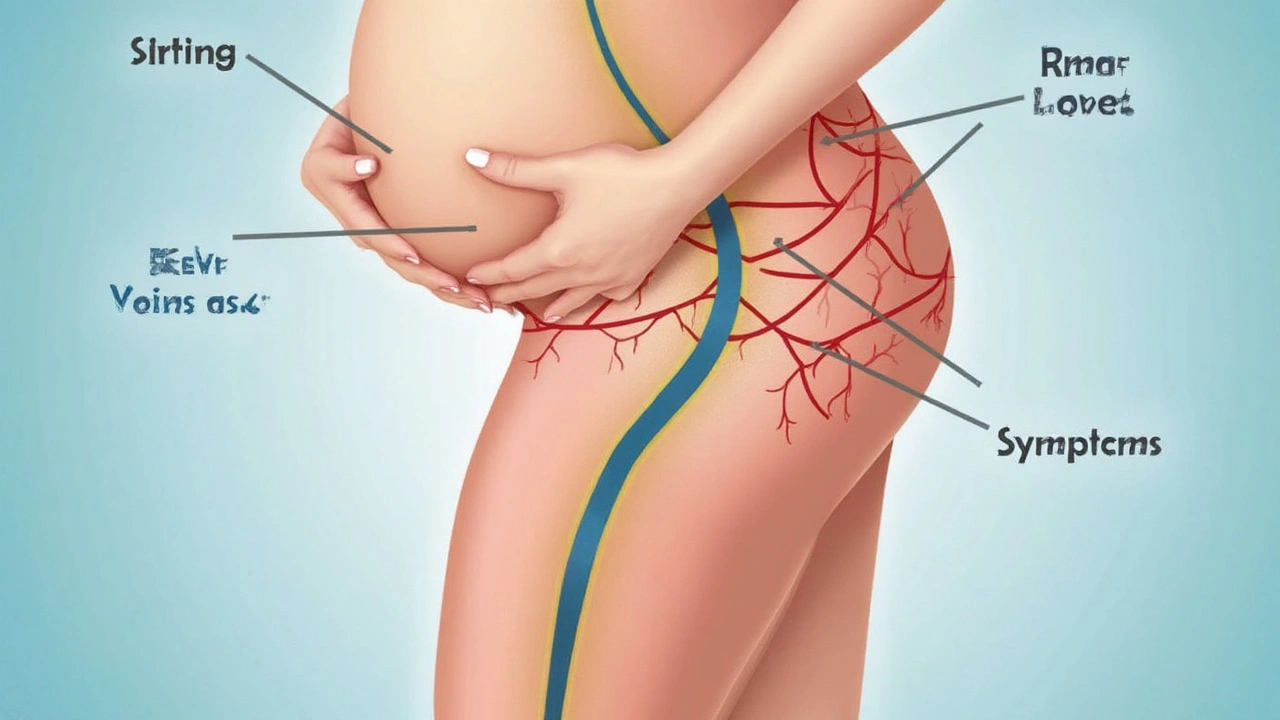
Let’s break it down: pregnancy flips more than just your sleep schedule. Behind-the-scenes, your body gears up for possible blood loss during delivery by turning your blood into something closer to gravy than water. This ‘hypercoagulable state,’ as the pros call it, means your system revs up the ability to form clots—nature’s way of protecting you from hemorrhage. But there’s a tradeoff. That added stickiness makes it easier for a blood clot to crop up in places it shouldn’t, like the deep veins in your legs or pelvis.
If you want numbers, here are some: about 1 in every 1,000 pregnant women develop a serious blood clot, compared to 1 in 10,000 non-pregnant young women. That’s a tenfold leap. Studies from the CDC have shown that most of these clots—about 80%—happen in the deep veins of the leg or pelvic area. These are called deep vein thrombosis, or DVT. The real nightmare scenario is when these clots break loose and hitchhike to the lungs, triggering a pulmonary embolism. That’s life-threatening and rapid-response time is critical.
You might be wondering who’s most at risk. Separate research has nailed down some red flags. The risk climbs higher if you have underlying problems like inherited clotting disorders (think Factor V Leiden), previous clots, obesity, age over 35, or if you’re expecting multiples. Bed rest—sometimes prescribed for high-risk pregnancies—can backfire by causing blood to pool in the legs. Even something as common as a C-section doubles your odds of clotting within the first six weeks after delivery compared to vaginal birth.
Why does your body go through all this? Evolution is partly to blame. The shift helps mothers survive childbirth—a time when bleeding out was a bigger threat than clots. But now, with advanced medicine, that natural edge sometimes backfires. Hormones, especially estrogen, also rewrite the clotting script. Add the pressure your growing belly puts on the veins in your pelvis, slowing blood return, and you’ve almost set the stage for DVT.
Warning Signs and Symptoms: What to Look Out For
You don’t need a medical degree to watch for DVT or pulmonary embolism, but you do need to know what’s worth calling the doctor over. Blood clots can be sneaky—sometimes, you’ll feel fine until a minor ache escalates. Watch for swelling in one leg that’s not matched by the other, unexplained warmth or redness on your calf or thigh, and pain that gets worse when you stand or walk. These are classic hints a DVT might be forming. Doctors often say, if one leg blows up like a balloon and feels tight, it’s a must-check.
So, what about clots in the lungs? Pulmonary embolism (PE) often comes out of nowhere. Sudden shortness of breath, chest pain (especially when you take a deep breath), or a fast heartbeat should all trigger alarm bells. If you get dizzy, faint, cough up blood, or feel like you’re having a panic attack for no real reason, don’t brush it off. About 15-24% of maternal deaths from PE occur within the first hour of symptoms. You don’t get a second chance if you ignore the signs.
Here’s a quick tip: symptoms of PE often mimic other pregnancy complaints, like shortness of breath, so trust your gut. If something doesn’t feel right or it’s worse than you’d expect for stage of pregnancy, speak up. Statistically, the biggest risk window stretches from the last trimester through six weeks postpartum. About half of clots show up after the baby is born, when the body is still in overdrive.
For reference, here’s a table showing the difference between common pregnancy discomforts and blood clot warnings:
| Symptom | Normal Pregnancy | Possible Blood Clot |
|---|---|---|
| Leg Swelling | Mild, both legs | Severe, one leg only |
| Pain | Dull, goes away with rest | Sharp, gets worse standing/walking |
| Breathlessness | Gradual, predictable | Sudden, unexplained |
| Heart Rate | Slightly fast | Very rapid, irregular |
| Redness/Warmth | Rare | Localized, only one spot |
If you see any matches in the right column, skip web searches and get medical care fast.
Proven Prevention Strategies: Staying a Step Ahead
No one wants to be the person worrying about blood clots every day, but a few practical steps can cut your risk. The simplest? Move as much as you safely can. Anything that keeps blood flowing—walking, stretching, flexing your legs if you’re stuck in bed or on a plane—helps. Doctors often recommend taking a stroll every hour, especially on those long flights or car trips. Compression stockings aren’t stylish, but research shows they work. They support your veins and nudge blood back toward the heart.
For those with more serious risk factors—like a personal or strong family history of clots, thrombophilia, or who have to do long stretches on bed rest—your care team might get proactive with blood-thinning medications. Low molecular weight heparin is the go-to. It doesn’t cross the placenta, so it’s safe for the baby. But these shots aren’t doled out to everyone; doctors tailor the plan depending on how many boxes you tick on the risk list.
Hydration is underrated. Thick, sticky blood loves dehydration. Aim for 8-10 glasses of water a day unless your doctor says otherwise. Play it cool with heat—no hot tubs or saunas, since heat dilates veins and can up your risk. Smoking is basically pouring gasoline on the fire; it damages your blood vessels and ramps up clot probability even more. If you’re struggling to quit, ask for help—no one expects you to go it alone.
Manage weight gain right on target. Obesity doubles or even triples clot risk in pregnancy. Use your doctor’s recommendations to keep things on track. And after a caesarean section or complicated delivery, don’t be shy about asking for early mobilization or mechanical devices that help blood move (like pneumatic compression boots). Hospitals use them for a reason—they work.
Here’s an at-a-glance list of strategies to lower your odds:
- Get moving—walk, stretch, and avoid sitting too long.
- Use compression stockings if advised.
- Stay hydrated—keep a water bottle close.
- Quit smoking—ask for support if you need it.
- Keep weight gain within your doctor’s guidelines.
- Get quick postpartum checkups, especially if you had a C-section.
- Take blood thinners only if prescribed, and follow your dose to the letter.
Want specifics? After a C-section, starting to walk within 12 to 24 hours drastically cuts your risk of DVT. If you’re traveling more than four hours, get up and stretch every hour, and don’t cross your legs for long. Studies by the Royal College of Obstetricians and Gynaecologists show women with inherited thrombophilia have up to a 10% chance of clotting during pregnancy unless given preventive medication. Don’t skip appointments—most doctors will screen you early for risk factors, but it helps to double-check and ask questions. Your voice can catch something they missed.
Frequently Asked Questions and Practical Advice
Got burning questions? You’re not alone. Lots of pregnant women worry that harmless things like bruises or leg cramps mean something worse, but know this: not all aches are clots. True DVT pain usually doesn’t shift with movement or rest. And while cramps often come and go, clot pain sticks around and gets sharper over time.
Can exercise cause a clot? Regular, moderate exercise is actually preventive, unless you have a known bleeding disorder or your doctor says to avoid it. Swimming, walking, and gentle prenatal yoga are all thumbs-up. High-intensity workouts or anything that involves heavy straining should be cleared first, especially if your risk is high. On the other hand, sitting still—binge-watching shows for days or being on bed rest without any movement—is much more dangerous for your blood flow.
If your doctor says you need blood thinners, what should you watch out for? Bruising is common, but if you start to see black stools, severe headaches, nosebleeds that won’t stop, or unexplained bruising, call your healthcare team right away. Don’t mix in over-the-counter NSAIDs (like ibuprofen) unless your doctor gives the green light—those can increase bleeding risks on top of what you’re already managing.
Travel is another big concern. If you have to fly, pack loose clothes, wear compression socks, drink water, and request an aisle seat for easier movement. Prop your feet up when possible, and use the footrest to keep the blood moving.
A lot of women ask about diet. There isn’t a magic food that melts away clots, but eating plenty of fruits, veggies, whole grains, and lean protein helps keep your blood healthy and reduces inflammation. If you’re on blood thinners, ask about vitamin K-rich foods—consistency is key since swings in K can affect medication levels.
You should also know that some groups need extra vigilance—women with lupus, sickle cell disease, severe varicose veins, or those using IVF are all at higher risk and should push for more screening.
And finally, don’t ignore follow-ups. The first six weeks after birth remain risky for clot formation, so keep your appointments. If anything feels off—even after you bring home your baby—it’s still worth mentioning to your provider.
It doesn’t have to be a guessing game. Blood clot risks in pregnancy are real, but steps like movement, hydration, weight control, and knowing the warning signs go a long way. Most women go through pregnancy without ever facing a clot, but blood clot in pregnancy is the keyword to remember because spotting it early can make all the difference for you and your baby.


ka modesto
June 15, 2025 AT 11:30Just had my second kid and didn’t know any of this until my OB mentioned it during a routine checkup. Seriously, this post should be mandatory reading for every pregnant person. Compression socks felt silly at first, but I wore them on my 8-hour flight home from Vegas and honestly? No swelling at all. Also, hydration is non-negotiable-I carry a 32oz bottle everywhere now. Even my cat knows when I’m low on water. 🐱💧
Holly Lowe
June 17, 2025 AT 08:55OMG YES. I was the girl who thought ‘blood clots’ were something that happened to grandpas in hospital dramas. Then I got DVT at 32 weeks and spent three days in the ER while my husband cried in the corner. My legs looked like overcooked sausages. I didn’t even realize it was a clot until my nurse said, ‘Honey, that’s not normal swelling.’ Now I’m an advocate. Move. Drink. Don’t sit. And if your doctor brushes you off? Find a new one. Your life isn’t a suggestion-it’s a priority. 💪❤️
dayana rincon
June 18, 2025 AT 03:10So basically pregnancy turns your body into a slow-motion horror movie where the villain is your own blood? 🤡 I’m just here for the popcorn and the compression socks. Also, why is everyone suddenly acting like they’re in a medical documentary? I’m not a lab rat, I’m a human who just wants to nap without being lectured about my venous return. 😴🫠
Simran Mishra
June 18, 2025 AT 13:07I read this while nursing my 4-month-old and it hit me like a freight train. I never thought about how my body changed during pregnancy-how everything was working overtime just to keep me alive and the baby safe. I had mild swelling in one leg at 36 weeks, but I blamed it on standing too long at work. I didn’t realize it could be something dangerous until I saw the table comparing normal vs. clot symptoms. Now I tell every pregnant friend I know: don’t normalize pain. If your calf feels like it’s wrapped in concrete, don’t wait. Call. Even if it’s 2 a.m. I wish someone had told me this before. I feel guilty for not knowing. But now I know. And I’ll keep telling people. Because no one should have to learn this the hard way.
Cindy Burgess
June 20, 2025 AT 05:20While the article presents a compelling case for heightened vigilance regarding thromboembolic events in the peripartum period, it is regrettable that the tone often veers into sensationalism. The assertion that blood becomes ‘closer to gravy’ is not scientifically precise and may undermine the credibility of the otherwise well-researched content. Furthermore, the inclusion of emotive language such as ‘nightmare scenario’ and ‘hitchhike to the lungs’ is inappropriate for a medical advisory context. A more restrained, evidence-based approach would better serve the audience.
Tressie Mitchell
June 20, 2025 AT 19:35Let’s be real-this isn’t ‘prevention tips,’ it’s a guilt trip wrapped in a PowerPoint. If you’re not wearing compression socks, drinking 10 glasses of water, walking every hour, avoiding heat, quitting smoking, and tracking your vitamin K intake while also avoiding NSAIDs and C-sections? You’re basically a walking clot waiting to happen. And if you’re obese? Congrats, you’re a liability. I’m sorry, but not everyone has the luxury of being a wellness influencer with a personal trainer and a nutritionist on speed dial. This reads like a rich white woman’s checklist, not medical advice.
Sondra Johnson
June 22, 2025 AT 07:41I get where Tressie is coming from-this article can feel overwhelming, especially if you’re low-income, working two jobs, or don’t have access to prenatal care. But I also think Holly and Simran are right: this info can save lives. The problem isn’t the advice-it’s the system that makes it hard to follow. I’m a nurse, and I’ve seen women ignore leg swelling because they couldn’t get an appointment for weeks. So yes, move, hydrate, speak up-but let’s also push for better access to compression stockings, telehealth follow-ups, and paid postpartum leave so people aren’t choosing between rent and a doctor’s visit. Knowledge is power, but access is justice.
Chelsey Gonzales
June 22, 2025 AT 07:53im so glad i read this bc i had a weird ache in my leg last week and i was like ‘eh its just pregnancy’ but then i thought about it and went to urgent care and they did an ultrasound and it was a tiny clot!! they gave me heparin and now im fine but i almost ignored it because i thought it was just cramps. yall. listen to your body. even if you think you’re being dramatic. i cried in the car after. i was so scared. but now i’m alive. and my baby is too. 💕
Orion Rentals
June 23, 2025 AT 20:05Thank you for the comprehensive overview. I would like to respectfully supplement the prevention section with a reference to the 2021 American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin No. 224, which recommends individualized risk assessment using validated tools such as the Padua Prediction Score or the IMPROVE VTE Risk Assessment Model. Additionally, while low molecular weight heparin remains the standard of care for high-risk patients, the bulletin notes that prophylactic dosing may be considered in moderate-risk patients with additional transient risk factors (e.g., prolonged immobilization postpartum). This nuanced approach may help mitigate over-treatment while preserving safety.