Anticoagulation Dosing Calculator for Kidney and Liver Disease
Patient Assessment
Anticoagulation Recommendation
Key considerations:
Dosing information:
When Your Kidneys and Liver Can’t Handle Blood Thinners
If you have both kidney disease and liver disease, taking a blood thinner isn’t like taking aspirin. It’s not a one-size-fits-all pill. The drugs that work fine for most people with atrial fibrillation can turn dangerous in someone with advanced organ damage. And yet, these patients are at the highest risk for strokes and clots. The question isn’t whether to anticoagulate-it’s how to do it safely.
Here’s the hard truth: most major studies on blood thinners like apixaban, rivaroxaban, and dabigatran deliberately left out people with severe kidney or liver disease. That means doctors are often guessing. No trial proved these drugs are safe in someone with an eGFR below 15 or Child-Pugh Class C cirrhosis. But that doesn’t mean you can’t treat them. It just means you have to be smarter about it.
How Kidney Disease Changes the Game
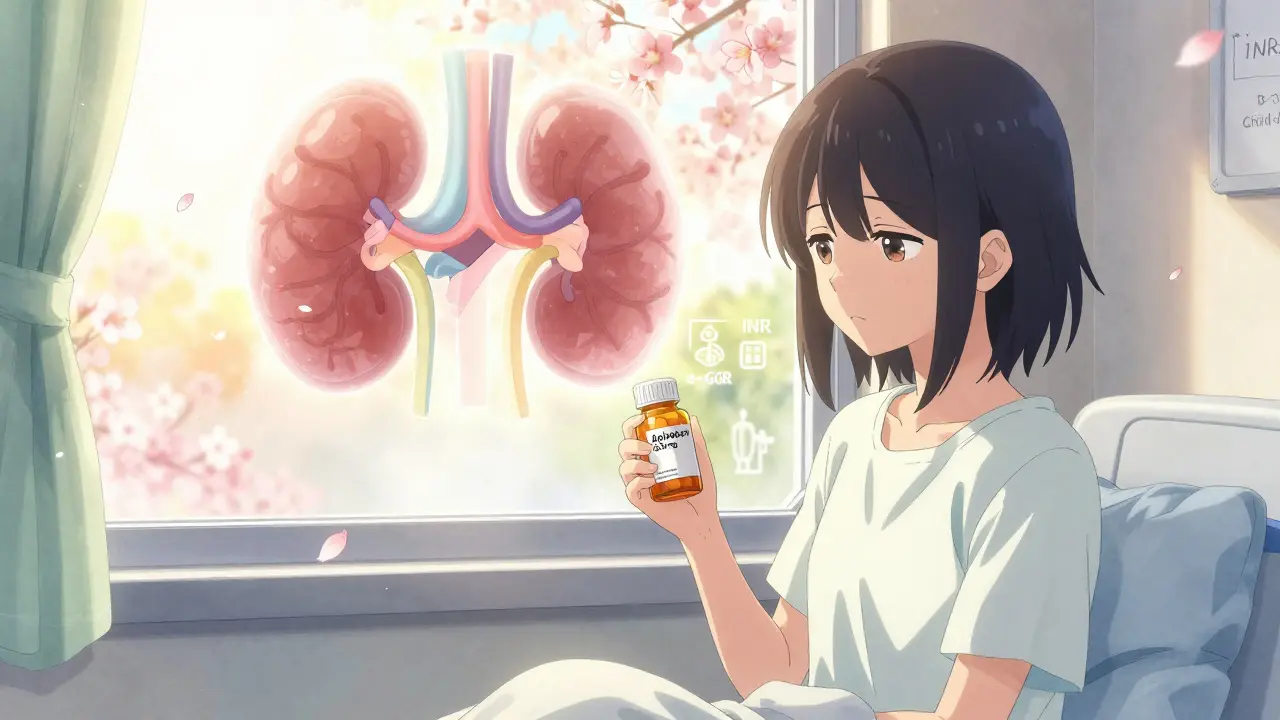
Your kidneys don’t just make urine-they clear drugs from your blood. When they fail, anticoagulants build up. That’s why dabigatran, which is 80% cleared by the kidneys, is banned in patients with eGFR under 30. Rivaroxaban and edoxaban also get risky below that level. But apixaban? It’s different. Only 27% leaves through the kidneys. That’s why, even in dialysis patients, it’s still used-carefully.
In stage 3b CKD (eGFR 30-44), you just cut the dose: apixaban drops from 5 mg to 2.5 mg twice daily. Rivaroxaban goes from 20 mg to 15 mg daily. Edoxaban from 60 mg to 30 mg. Simple, right? Not quite. Creatinine-based eGFR estimates are wrong up to 40% of the time in advanced kidney disease. A patient might look like they’re in stage 4, but their muscle mass is low from malnutrition, so their creatinine is artificially low. That’s why some nephrologists use cystatin C instead-or just watch trends over time.
For dialysis patients, the data is messy. One study found apixaban 2.5 mg twice daily gave blood levels around 47 ng/mL-less than half of what you’d see in healthy people. Yet, bleeding rates were lower than with warfarin. Another study showed rivaroxaban 10 mg daily reached 78 ng/mL. Still, the European guidelines say don’t use DOACs in dialysis. The American College of Chest Physicians says maybe use apixaban 5 mg daily. Why the conflict? Because no randomized trial has been done. Not yet.
Warfarin is still common in dialysis patients-63% of treated cases in one big registry. But INR monitoring becomes unreliable. Your liver can’t make clotting factors properly, so the INR might be high even if you’re not anticoagulated enough. That’s why some doctors aim for a lower target: 1.8-2.5 instead of 2.0-3.0. And they check INR every two weeks, not monthly.
Liver Disease: More Than Just an INR
Liver disease doesn’t just mess with drug clearance. It breaks your entire clotting system. Your liver makes clotting factors-and anticoagulant proteins too. So when it fails, you’re both more likely to bleed and more likely to clot. That’s why a cirrhotic patient with a low platelet count and high INR might still get a portal vein clot.
Child-Pugh scoring is your best friend here. Class A (score 5-6)? DOACs are probably fine at normal doses. Class B (7-9)? Use with caution. Reduce the dose. Class C (10+)? Avoid DOACs entirely. The RE-CIRRHOSIS study showed a 5.2-fold higher bleeding risk with DOACs in this group.
But here’s the twist: INR is useless in advanced liver disease. It only measures vitamin K-dependent factors. It ignores low fibrinogen, low platelets, and abnormal clot strength. That’s why some hepatologists use TEG or ROTEM-tests that show how your whole blood clots. But only 38% of U.S. hospitals have them. So what do you do? You look at the whole picture: platelet count, albumin, bilirubin, MELD score. If platelets are under 50,000/μL or MELD is over 20, many experts stop anticoagulation altogether.
Warfarin has a place here because we know how to reverse it. Vitamin K, fresh frozen plasma, prothrombin complex concentrate-they all work. But the problem? Keeping INR in range is a nightmare. One study found cirrhotic patients only spent 45% of their time in the therapeutic range. Healthy patients hit 65%. That’s a huge gap.
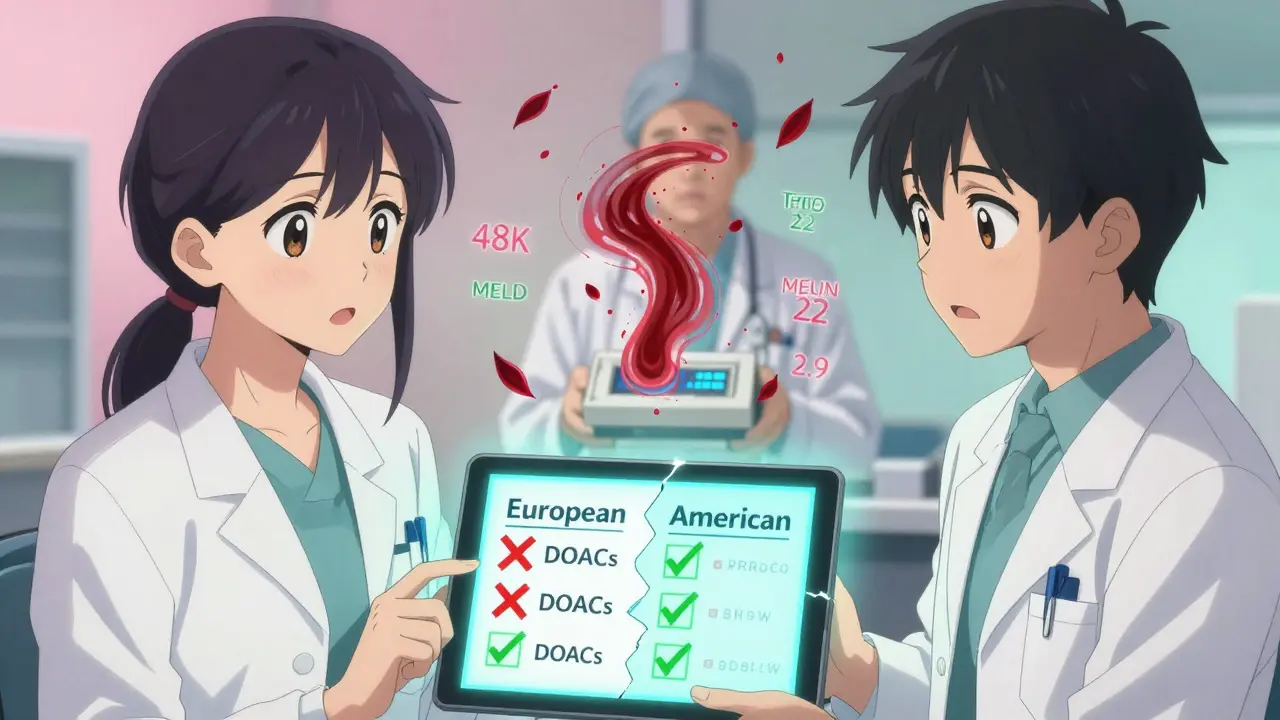
DOACs vs. Warfarin: The Real Numbers
Let’s cut through the noise. In patients with moderate kidney disease (eGFR 25-30), apixaban cuts major bleeding by 31% compared to warfarin. That’s huge. And in CKD patients, DOACs reduce brain bleeds by 62%. That’s the biggest win.
But in end-stage kidney disease? The data flips. For patients with mechanical heart valves, warfarin is still the only approved option. DOACs aren’t even studied here. And for those with a history of GI bleeding? Rivaroxaban is risky-2.8 times more GI bleeds than warfarin in dialysis patients. Apixaban? Better. But still not risk-free.
For liver disease, DOACs reduce intracranial bleeding too. But if you bleed in the abdomen? There’s no antidote for rivaroxaban or apixaban except andexanet alfa-and it costs $19,000 per dose. And only 45% of hospitals stock it. Idarucizumab (for dabigatran) is cheaper at $3,500, but useless if you’re not on dabigatran.
Real-world data from a 12,850-patient dialysis registry showed DOACs had fewer bleeds (14.2 vs. 18.7 per 100 patient-years) than warfarin. But strokes? Almost the same. That’s the trade-off: less bleeding, same stroke protection. For many, that’s worth it.
What Doctors Actually Do in the Real World
Here’s what you won’t find in guidelines: the messy, on-the-ground decisions.
A nephrologist in Texas told a Reddit thread he’s been giving apixaban 2.5 mg daily to 15 dialysis patients for two years. No bleeds. No clots. Another doctor in Ohio described a patient who had a massive retroperitoneal bleed on the same dose. Both used the same drug. Same dose. Same condition. One worked. One didn’t. Why? Maybe it was the GI bleed history. Maybe it was the low albumin. Maybe it was luck.
In liver disease, 41% of hepatologists check platelet function before starting anticoagulation. Why? Because a platelet count of 80,000 doesn’t mean the platelets work. Some cirrhotic patients have dysfunctional platelets that can’t stick together-even if the number looks okay.
Most clinics don’t have protocols for dual organ failure. A 2021 survey found 78% of U.S. hospitals lack written rules for anticoagulation in patients with both CKD and cirrhosis. That means decisions are made by whoever’s on call. And that’s dangerous.
When to Stop, When to Try, When to Wait
Here’s a simple decision tree, based on real-world practice:
- Is the patient on dialysis? If yes, avoid dabigatran and rivaroxaban. Apixaban 2.5 mg twice daily is the safest bet-if no GI bleed history. If there’s a history of GI bleeding? Stick with warfarin and target INR 1.8-2.5.
- Is the liver disease Child-Pugh C? Avoid all DOACs. Use warfarin only if absolutely necessary (like a recent portal vein clot), and monitor closely. Consider no anticoagulation if bleeding risk is too high.
- Is the patient in stage 4 or 5 CKD with Child-Pugh B? This is the gray zone. Consult nephrology and hepatology together. If you must anticoagulate, use apixaban 2.5 mg twice daily. Check platelets and MELD monthly. Stop if platelets drop below 50,000 or MELD rises above 20.
- Is this for stroke prevention in AF? Then CHA₂DS₂-VASc score matters. If it’s 3 or higher, the stroke risk usually outweighs the bleeding risk-even in advanced disease.
- Is this for a portal vein clot? Then you’re treating a life-threatening clot, not just preventing one. Bleeding risk is secondary. Many experts will use DOACs even in Child-Pugh B if the clot is recent and growing.
What’s Coming Next
Two big trials are underway. The MYD88 trial is comparing apixaban to warfarin in 500 dialysis patients. Results in 2025. The LIVER-DOAC registry is tracking 1,200 cirrhotic patients on DOACs worldwide. We might finally get real answers.
The FDA is preparing new labeling for apixaban in end-stage kidney disease. KDIGO is updating its guidelines in late 2024. And hospitals? They’re slowly starting to build protocols. But right now, the best tool you have is not a guideline-it’s a conversation. Between nephrologist, hepatologist, cardiologist, and patient.
There’s no perfect answer. Only the least bad one. And sometimes, that’s still better than doing nothing.
Can I take apixaban if I’m on dialysis?
Yes, but only at a reduced dose: 2.5 mg twice daily. This is based on pharmacokinetic data and real-world outcomes showing lower bleeding risk compared to warfarin. Avoid apixaban if you have a history of gastrointestinal bleeding. Never use dabigatran or rivaroxaban in dialysis patients.
Is warfarin safer than DOACs in liver disease?
Not necessarily. DOACs reduce the risk of brain bleeds, which are more deadly. But in Child-Pugh C cirrhosis, DOACs are linked to much higher bleeding risk. Warfarin can be used with caution, but INR is unreliable. Reversal agents are available, but maintaining therapeutic INR is hard. The choice depends on bleeding history, platelet count, and clot risk.
Why is INR not reliable in liver disease?
INR only measures vitamin K-dependent clotting factors (II, VII, IX, X). In advanced liver disease, you also have low fibrinogen, low platelets, and abnormal clotting proteins. A high INR might mean you’re not clotting enough-or it might just mean your liver is failing. That’s why tests like TEG or ROTEM, which measure overall clot strength, are better but rarely available.
What’s the best anticoagulant for someone with both kidney and liver disease?
Apixaban at 2.5 mg twice daily is the most studied and safest option in this group. It’s less dependent on kidney clearance and has lower bleeding rates than warfarin in moderate CKD. But if liver disease is severe (Child-Pugh C), avoid DOACs entirely. Always involve both nephrology and hepatology before starting.
Can I use DOACs if I have a low platelet count?
Platelets under 50,000/μL are a red flag. Low platelets increase bleeding risk, especially in liver disease. Many experts stop anticoagulation at this level. If you must treat, use the lowest possible DOAC dose and monitor platelets weekly. Consider TEG/ROTEM if available to assess clot function, not just count.
What should I do if I start bleeding while on a DOAC?
Stop the drug immediately. Call emergency services. For dabigatran, use idarucizumab (Praxbind®). For apixaban or rivaroxaban, use andexanet alfa (Andexxa®)-if available. If not, give activated charcoal (if recent dose), prothrombin complex concentrate (PCC), and consider tranexamic acid. Supportive care matters more than reversal agents in most cases.

Donna Fleetwood
January 31, 2026 AT 05:07Sheila Garfield
February 1, 2026 AT 22:04calanha nevin
February 2, 2026 AT 00:39Amy Insalaco
February 3, 2026 AT 22:50